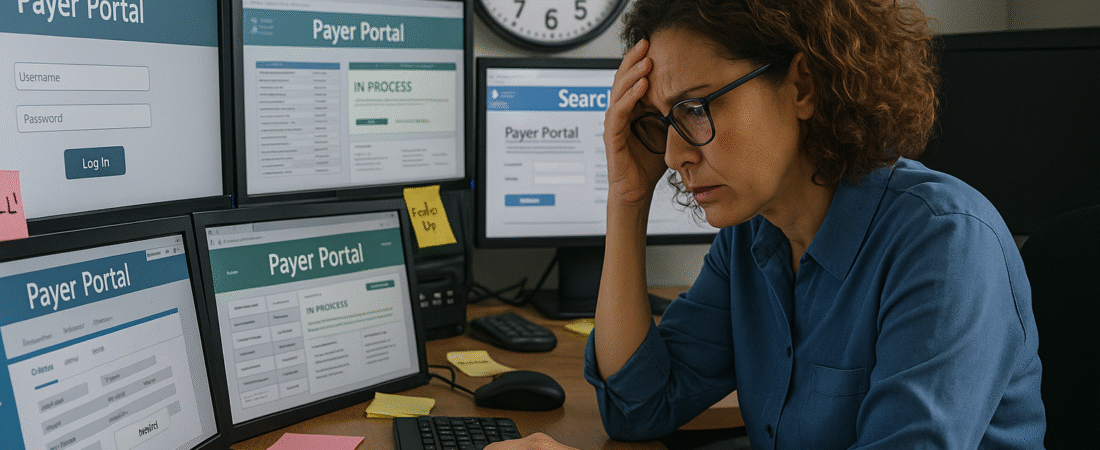
Payers promise transparency and efficiency through their online portals, APIs, and dashboards—but the reality for billing teams is often the opposite. Rather than streamlining workflows, the proliferation of payer-specific tools creates friction, data silos, and duplicated effort. The result? Portal paralysis—when your team is logging into dozens of systems a day, but still not getting the answers they need.
The Problem Isn’t Access—It’s Overload:
In theory, payer portals should make it easier to check claim status, retrieve remits, submit appeals, and verify eligibility. But with each payer offering a different interface, logic, and terminology, your staff ends up navigating a labyrinth of logins, menus, and inconsistent data.
Examples of common inefficiencies include:
- No centralized dashboard: Teams must log into 10+ portals daily to track claims across payers.
- Data mismatch: What appears as “pending” in one portal may be marked “in process” in another—with no clear explanation or resolution path.
- Fragmented documentation: EOBs, attachments, and appeal forms live in separate tabs or systems, requiring staff to download and manually merge information.
- Staff training overload: New team members must learn the quirks of each payer interface—slowing onboarding and increasing error risk.
What It’s Costing Your Practice:
This portal proliferation not only drains productivity—it increases aging AR, delays appeals, and leads to missed follow-ups. Without a system to aggregate or standardize information across payers, even experienced billing teams spend more time chasing data than solving problems.
And for smaller practices or stretched billing teams, the problem compounds quickly. You’re not just managing claims—you’re managing systems that don’t talk to each other.
What Progressive RCM Teams Are Doing Instead:
To overcome portal paralysis, top-performing organizations are shifting their approach from passive portal use to intentional aggregation and automation. That includes:
- Using clearinghouse tools or bolt-on AI assistants to consolidate payer information into one searchable interface.
- Mapping each portal’s terminology to internal workflows so “in process” or “information needed” isn’t left to interpretation.
- Embedding payer-specific logic into task queues, so staff are assigned work by claim status—not payer system.
- Reducing logins with credential management tools and portal shortcut hubs to speed up daily navigation.
How Thrive Helps You Navigate the Maze:
At Thrive Revenue Cycle, we’ve helped clients replace multi-portal chaos with simplified, centralized dashboards tailored to their payer mix. Whether we’re designing a portal usage protocol or integrating clearinghouse functionality, we focus on reclaiming your team’s time—and eliminating the guesswork.
Our clients have reduced redundant logins by up to 60%, while improving claim follow-up rates and reducing AR over 90 days.
Conclusion:
The solution to payer portal chaos isn’t to stop using the tools—it’s to use them strategically. With the right workflows, technology, and guidance, you can turn fragmented access into functional oversight. Because chasing claims shouldn’t feel like chasing your tail.