Your cart is currently empty!
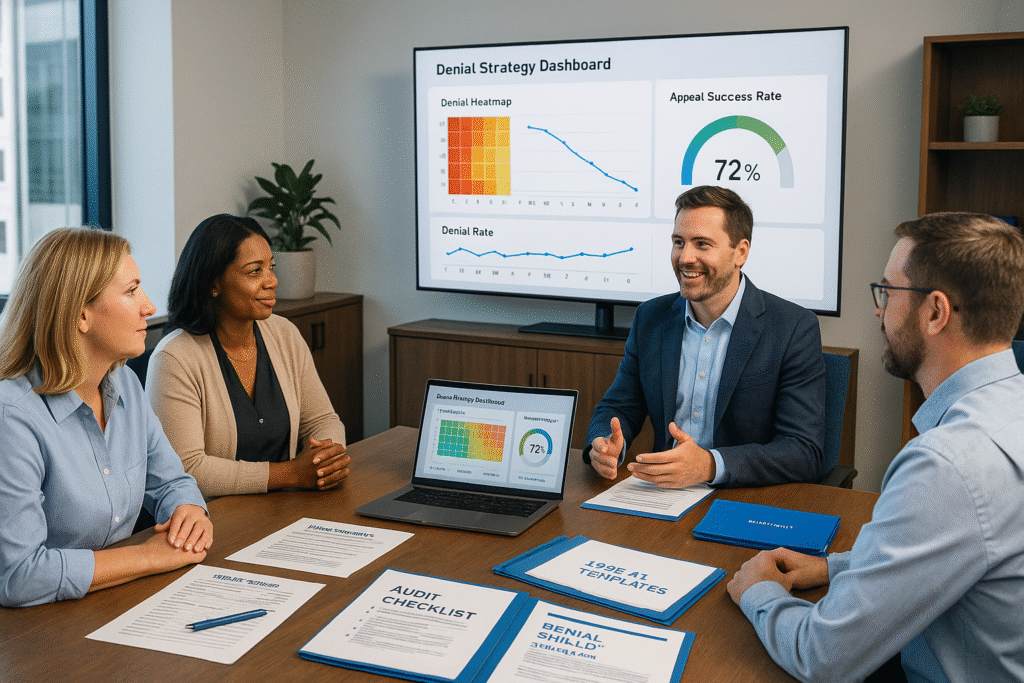
📊 Denial Strategy Partnership™
Turn denial patterns into predictable revenue recovery.
High denial rates aren’t just a billing problem—they’re a recurring revenue leak. The Denial Strategy Partnership™ combines advanced denial analytics, proven appeal strategies, and ongoing advisory support to stop revenue loss at the source.
We don’t just help you fight denials—we help you prevent them.
Denials Are Draining Your Bottom Line
- Payer rules change without warning
- Modifiers, prior auths, and eligibility errors slip through
- Patterns in denials go unnoticed until cash flow suffers
- Appeals are reactive instead of proactive
- The same denials keep coming back month after month
From Data to Action in 90 Days or Less
With the Denial Strategy Partnership™, you get a dedicated denial prevention team without adding payroll:
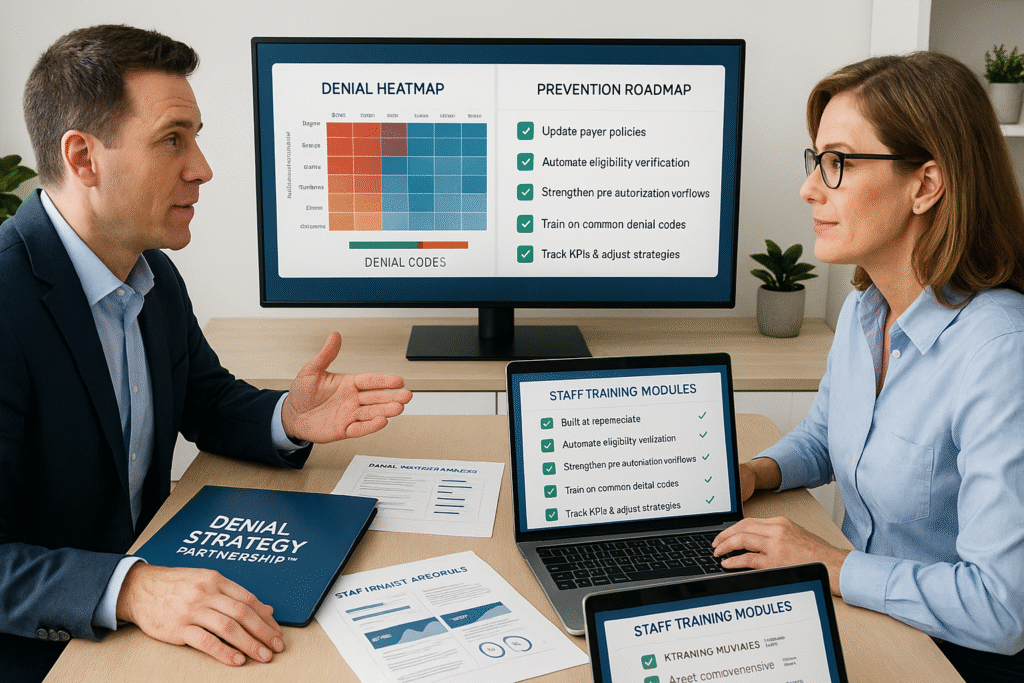
- Advanced Denial Pattern Analysis — Identify root causes with heatmaps, payer-specific trends, and code-level data.
- Appeal Shield™ Integration — Use proven, payer-specific appeal templates to recover revenue faster.
- Prevention Roadmap — Implement policy, workflow, and training updates to keep denials from returning.
- Ongoing Monitoring & Coaching — Monthly denial metrics review and staff guidance.
- Custom KPI Tracking — Built-in reporting so you see results in real time.
What’s Included in Your Partnership
- 📊 Quarterly Denial Heatmap & Root Cause Analysis
- 🛡️ Appeal Template Access by payer, specialty, and denial type
- 📂 Customized Denial Prevention Plan
- 🧠 Staff Training Modules on denial prevention best practices
- 🔍 Live Monthly Review Call with your denial strategist
- 🗂️ Annual Workflow Audit to maintain prevention gains
Pricing Options
Quarterly Partnership: $1,250 every 3 months
- Full analysis + monthly coaching
- Access to all templates & reports
Annual Partnership: $4,500 per year (save 10%)
- All quarterly benefits
- Annual comprehensive workflow & compliance review
Who This Is For
- Multi-specialty clinics with recurring payer denials
- Rural health centers with small billing teams
- Practices that appeal but can’t reduce repeat denials
- Any organization wanting predictable cash flow from clean claims
Why Choose This Over a One-Time Fix?
- Continuous monitoring catches issues before they escalate
- Eliminates the “fire drill” approach to denials
- Builds internal denial prevention expertise
- Measurable improvement in cash flow and staff efficiency
Comparison Block: One-Time Service vs. Partnership
| Feature | One-Time Denial Audit | Denial Strategy Partnership™ |
|---|---|---|
| Denial pattern analysis | ✅ | ✅ |
| Payer-specific appeal templates | ✅ | ✅ |
| Prevention plan | ✅ | ✅ |
| Monthly coaching calls | ❌ | ✅ |
| Ongoing KPI tracking | ❌ | ✅ |
| Annual workflow audit | ❌ | ✅ |
| Continuous prevention & improvement | ❌ | ✅ |
Make Denials a Thing of the Past
Every denied claim is lost cash flow and wasted staff time. With the Denial Strategy Partnership™, you get a repeatable, data-backed system to prevent denials, win appeals, and protect your revenue long-term.
