Your cart is currently empty!
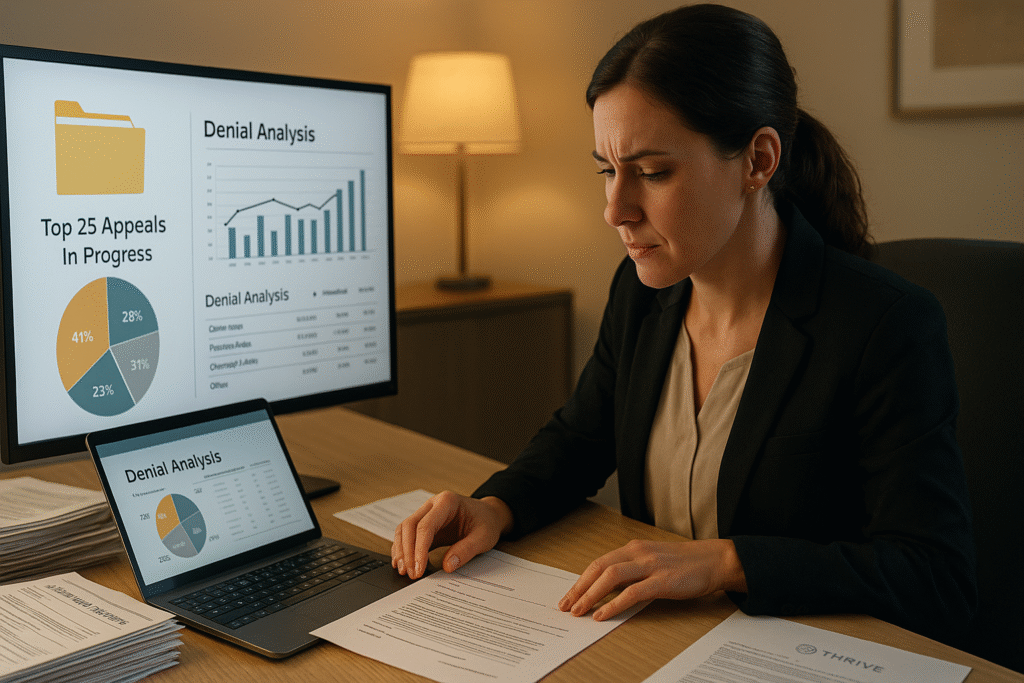
Denial Audit & Appeals Campaign – Strategic Oversight for Revenue Recovery & Risk Prevention
💲 Price: $3,500 (One-time)
Overview
Denied claims are one of the largest sources of preventable revenue loss for healthcare providers—yet many are never appealed. Thrive’s Denial Audit & Appeals Campaign offers a turnkey solution to uncover the why behind your denials, launch targeted appeals, and build long-term prevention strategies. We don’t just appeal—we help eliminate the need to.
Ideal for practices overwhelmed by rejections, short-staffed billing teams, or those transitioning to new systems or payers.
What’s Included
- Review of 90 days of denied claims (commercial, Medicare, Medicaid)
- Categorization by denial type, payer, CPT/ICD mismatch, documentation, etc.
- Root-cause analysis to identify trends and process breakdowns
- Up to 25 custom appeal letters written and submitted
- Denial prevention checklist and payer-specific tips
- Final Denial Audit Report with analytics, success rates, and recommendations
How It Works
- After purchase, you’ll complete a secure intake form and upload denial logs and EOBs.
- Thrive analyzes the data, prioritizing high-dollar/high-likelihood appeals.
- We draft and submit up to 25 formal appeals on your behalf using payer-specific protocols.
- You receive a detailed final report with denial trends, appeal results, and training opportunities.
ROI & Benefits
- Recover lost revenue from denied claims (typical recovery: $25K–$100K)
- Identify preventable denial patterns (e.g., modifiers, eligibility, timing)
- Gain a ready-to-use appeals letter library
- Reduce AR and improve first-pass claim rate
- Empower staff with a clearer path to clean claims
Timeline & Delivery
- Review and appeals completed in 10–14 business days
- Delivery: PDF report + appeal letter documentation
- Option to purchase additional appeals as an add-on ($500 per 10 appeals)
Compliance Note
Thrive operates under HIPAA-compliant workflows and signs a Business Associate Agreement (BAA) with every client. All PHI is encrypted in transit and at rest.
