Protect Revenue from Day One
Turnkey toolkit for provider enrollment and payer onboarding — so your team avoids delays, tracks every step, and stays compliant from the start.
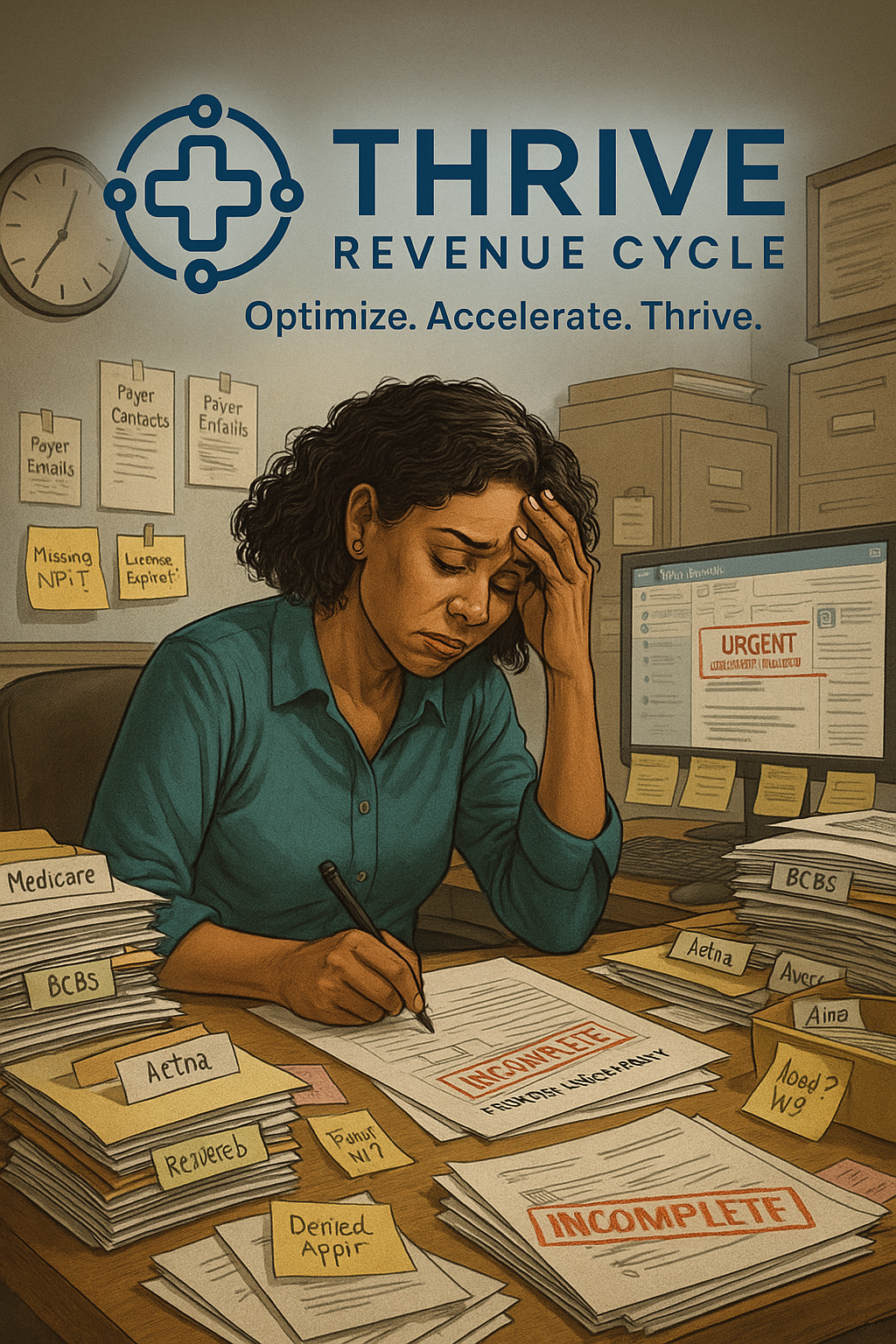
The Reality for Most Practices
Delayed credentialing = delayed revenue.
- Small errors in enrollment cause months of lost income
- Sticky notes, emails, and spreadsheets = blind spots
- Missed steps force rework, denials, or backdated start dates
- Admin teams waste hours chasing statuses across payers
- Medicare, Medicaid, and commercial plans all have different rules — and no room for mistakes
Without a centralized system, providers lose money before they ever see a patient.
When to Choose The Credentialing Guard™
✅ You’re onboarding new providers or expanding locations
✅ You don’t have a dedicated credentialing coordinator
✅ You want one dashboard for every payer, provider, and status
✅ You need compliance-aligned workflows from day one
The Cost of Not Acting
⚠ Delayed revenue while waiting for payer enrollment
⚠ Increased denials tied to incorrect or incomplete credentialing
⚠ Extra staff time reworking applications
⚠ Compliance risk from missing Medicare, Medicaid, or commercial payer requirements

Meet The Credentialing Guard™
The Credentialing Guard™ is a digital toolkit built to centralize, standardize, and simplify the payer enrollment process.
You’ll get a fully editable tracker, policy-aligned checklists, and prewritten templates—plus optional access to a credentialing expert to help set everything up.
How It Helps RCM & Operations Leaders
📊 Track Every Payer – Central dashboard for enrollments
🧠 Prevent Errors – Checklists mapped to every step
🕒 Save Time – No more digging through emails
💰 Start Revenue Faster – Avoid backdated effective dates
⚖ Stay Compliant – Aligned with CAQH, CMS, and commercial payers
What’s Included
Credentialing Guard™ Essentials – $249 One-Time
✔ Editable Credentialing Tracker (Excel/Sheets)
✔ Checklist Bundle (NPI, CAQH, Medicare, Medicaid, BCBS, Commercial)
✔ Templates & Forms (Attestations, scripts, email templates)
✔ Timelines & Policy Snapshot (Processing timelines + compliance callouts)
✔ Quick Start Guide (Escalation paths, payer-specific tips)
Credentialing Guard™ + Expert Boost – $399 One-Time
Everything in the Toolkit plus:
✔ 30-Minute Coaching Call with a Credentialing Expert
✔ Real-time setup review and workflow troubleshooting
✔ Q&A for payer-specific roadblocks and edge cases
Results You Can Expect
✅ Faster onboarding for new providers
✅ Reduced errors and rework in credentialing submissions
✅ Clear, centralized tracking across payers and providers
✅ Compliance from the first step, not the last

“We thought our billing delay was coding—but it was credentialing. This toolkit showed us the gaps and gave our admin staff the clarity they needed.”
Mary Jo L
RCM Manager
What’s Inside
Whether you’re just starting with provider onboarding or need expert eyes on a complex enrollment mess, The Credentialing Guard™ has you covered.
Choose the Essentials Toolkit to streamline your credentialing process with plug-and-play trackers, templates, and checklists — or level up with the Expert Boost, which adds a 1:1 consult to help you troubleshoot bottlenecks, customize your workflows, and fast-track your results.
No subscriptions. No fluff. Just the tools and support your team needs to protect revenue and reduce credentialing risk — from day one.
Toolkit to track enrollments, avoid errors, and streamline onboarding from day one
Everything you need to stay compliant and onboard faster
Credentialing Guard™ + Expert Boost
Everything in Essentials, plus a 30-minute credentialing consult to optimize your setup
Toolkit + 1:1 credentialing guidance from a Thrive advisor
Zero-Risk Guarantee
If The Credentialing Guard™ doesn’t help you track and complete payer enrollments more efficiently within 30 days, we’ll credit your full purchase toward any other Shield™ product or service. No questions asked.
