Latest posts
-
Escalation Fatigue: Why Your AR Team Can’t Get Through to Payers Anymore
If your AR team spends more time on hold than resolving issues—or if they’re constantly being transferred, disconnected, or “call back later-ed”—you’re not alone. Payers have made it increasingly difficult to escalate inquiries, resolve claim holds, or even speak to a human. The result? Escalation fatigue: a costly blend of burnout, delays, and avoidable write-offs.…
-
Under the Radar: How Small Denials Add Up to Big Losses
It’s easy to focus your team’s energy on the big-ticket denials—high-dollar claims that demand attention. But while those denials are obvious, what’s often overlooked are the low-dollar, low-effort denials that quietly accumulate and slowly drain your revenue. The $15 here, the $42 there—they may seem insignificant in isolation, but across a month or quarter, these…
-
⏳ Silent Denials: When Payers Don’t Respond and A/R Explodes
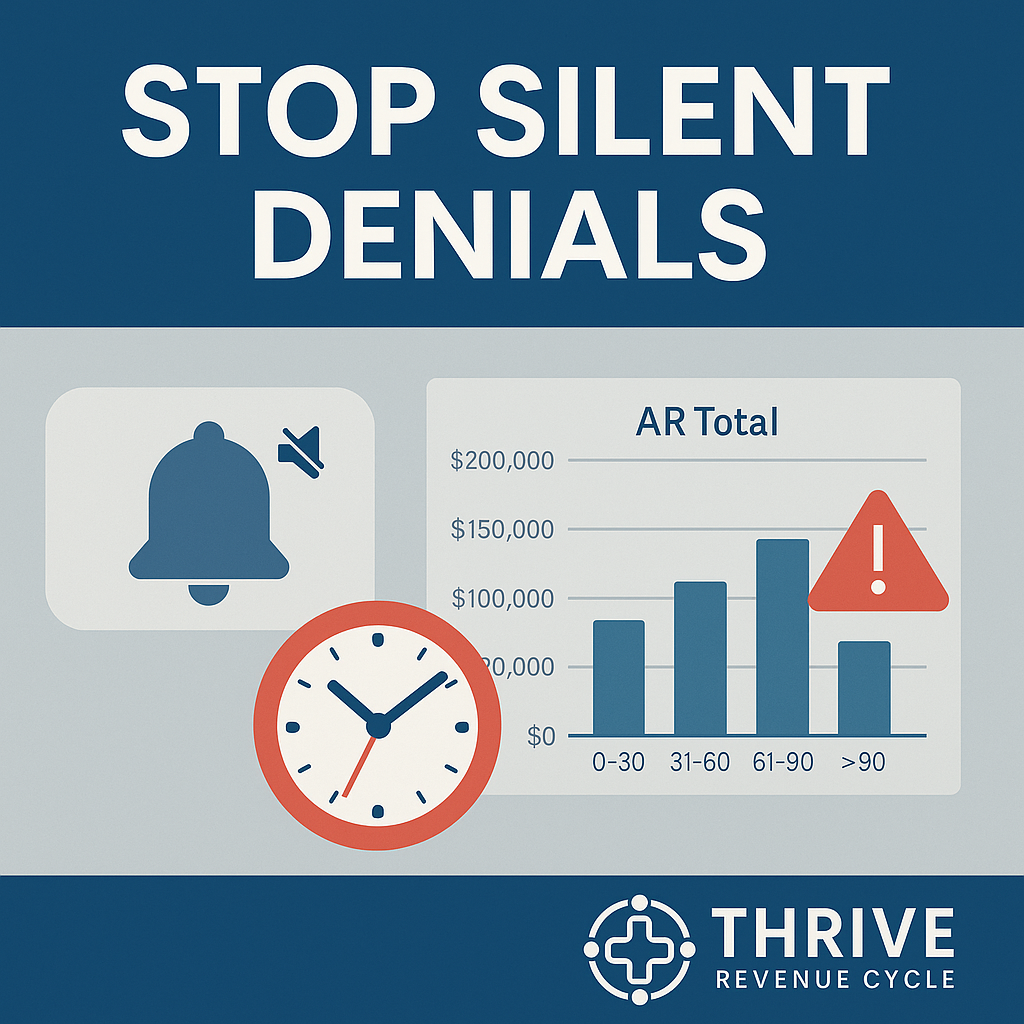
What Are Silent Denials? Unlike formal denials that generate an Explanation of Benefits (EOB) or denial code, silent denials happen when payers simply don’t respond.The claim isn’t processed, isn’t rejected, and isn’t marked as pending. It just… sits there. Why? Silent denials are dangerous because they: The True Cost of Non-Response Every week that a…
-
Portal Paralysis: When Too Many Payer Tools Create More Confusion Than Clarity
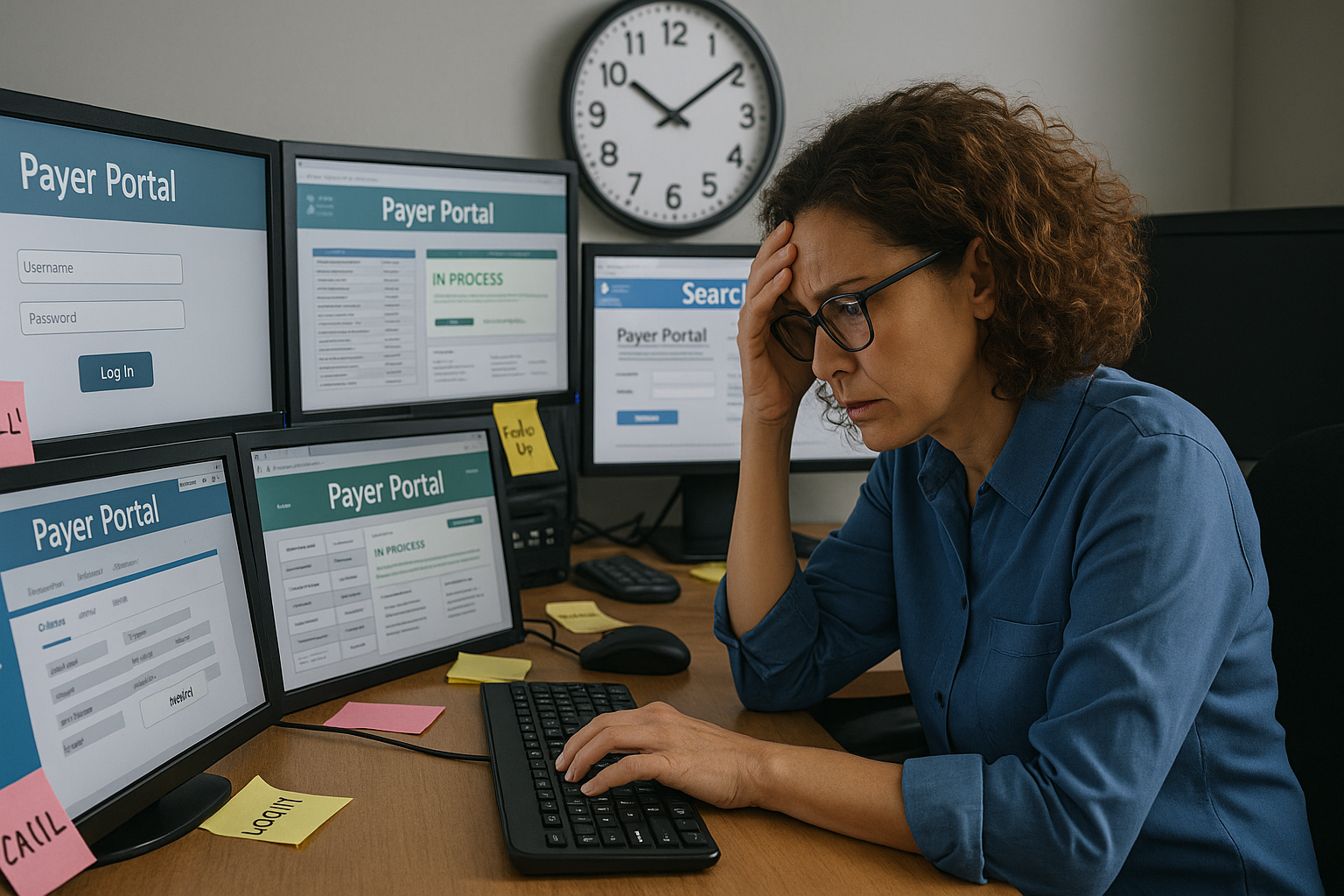
Payers promise transparency and efficiency through their online portals, APIs, and dashboards—but the reality for billing teams is often the opposite. Rather than streamlining workflows, the proliferation of payer-specific tools creates friction, data silos, and duplicated effort. The result? Portal paralysis—when your team is logging into dozens of systems a day, but still not getting…
-
Appeals That Actually Win: Beyond Templates to Root-Cause Fixes

When Copy-Paste Appeals Stop Working Two months ago, Jason, the revenue cycle director at a mid‑sized orthopedic practice, noticed a troubling trend. His team was sending appeal letters for denied claims faster than ever, using the same “tried‑and‑true” templates they’d relied on for years. But payer overturn rates were slipping—from 68% to just 41%. The…
-
The Credentialing Trap: How Delays at the Start Cripple Your Revenue Cycle

Credentialing is often treated as a standalone task—an administrative checklist that simply needs to be completed before a provider can see patients. But this mindset underestimates the far-reaching consequences of getting it wrong. When credentialing delays occur, the impact ripples downstream: denied claims, unbilled visits, and mounting frustration for patients and staff alike. More Than…
-
When Clean Claims Go Dirty: The Hidden Errors Sabotaging Your Reimbursements

The Day the Cash Flow Slowed to a Crawl Last summer, Maria, the practice manager of a busy rural cardiology clinic, was feeling confident. The team had just hit a 94% clean-claim submission rate—a figure that meant faster payments and fewer headaches. But by October, things had changed. Reimbursement timelines were stretching, denials were piling…
-
📌 Appeal or Abandon? A Data-Driven Framework for Smart Denial Triage

The Appeal Dilemma Denials are inevitable—but wasted appeals are optional.Many revenue cycle teams treat denials reactively: appeal everything, escalate if denied again, and hope something sticks. This approach is: Not all denials deserve your time. The question isn’t just can you appeal, but should you? Denial Volume ≠ Denial Value Denial rates get attention, but…
-
🩺 Time to Talk TAT: Why Turnaround Time Should Be a KPI in Your Revenue Cycle

What Is Turnaround Time — and Why Does It Matter? Turnaround time (TAT) refers to the time it takes for a task or process in the revenue cycle to be completed from start to finish. Whether it’s submitting a claim, receiving a payment, responding to a denial, or obtaining prior authorization — the speed of…
-
Template Trouble: How Poor EHR Design Is Killing Clean Claims in 2025

📉 Your EHR Isn’t Helping—It’s Hurting Your Claims EHR templates were designed to streamline workflows, standardize notes, and help providers meet documentation requirements faster. But in 2025, they’ve become a top source of hidden claim contamination. At Thrive, we’ve seen it firsthand: templates meant to speed things up actually introduce patterns that trigger payer audits,…
