Latest posts
-
🧾 The Front Desk Revenue Drain: How Inaccurate Data Entry Wrecks Clean Claims

First Impressions Matter—To Payers, Too The front desk is your patient’s first touchpoint—but it’s also where many revenue leaks begin. A misspelled name.An outdated insurance ID.A missing referral or authorization. These may seem like small clerical mistakes—but they cause big problems downstream. In fact, up to 80% of denied or rejected claims can be traced…
-
Too Many Hands: When Fragmented Billing Ownership Slows Down Reimbursement
Billing isn’t a single task—it’s a process with dozens of interdependent steps. But when too many people are responsible for too many pieces of that process, things start to slip. Claims get stuck in handoffs, accountability gets diluted, and cash flow suffers. If your team is constantly saying, “I thought someone else did that,” it’s…
-
Under the Radar: How Small Denials Add Up to Big Losses
It’s easy to focus your team’s energy on the big-ticket denials—high-dollar claims that demand attention. But while those denials are obvious, what’s often overlooked are the low-dollar, low-effort denials that quietly accumulate and slowly drain your revenue. The $15 here, the $42 there—they may seem insignificant in isolation, but across a month or quarter, these…
-
🏔️ Authorization Avalanche: Reducing Workflow Bottlenecks in Prior Authorization

The Prior Auth Problem Isn’t Going Away If you feel like getting a prior authorization approved takes longer than delivering care—you’re not alone. Payers are expanding PA requirements across diagnostics, radiology, physical therapy, surgical consults, and even standard medications. As a result: And most dangerously? Claims get denied when PAs aren’t filed—or not filed fast…
-
Portal Paralysis: When Too Many Payer Tools Create More Confusion Than Clarity
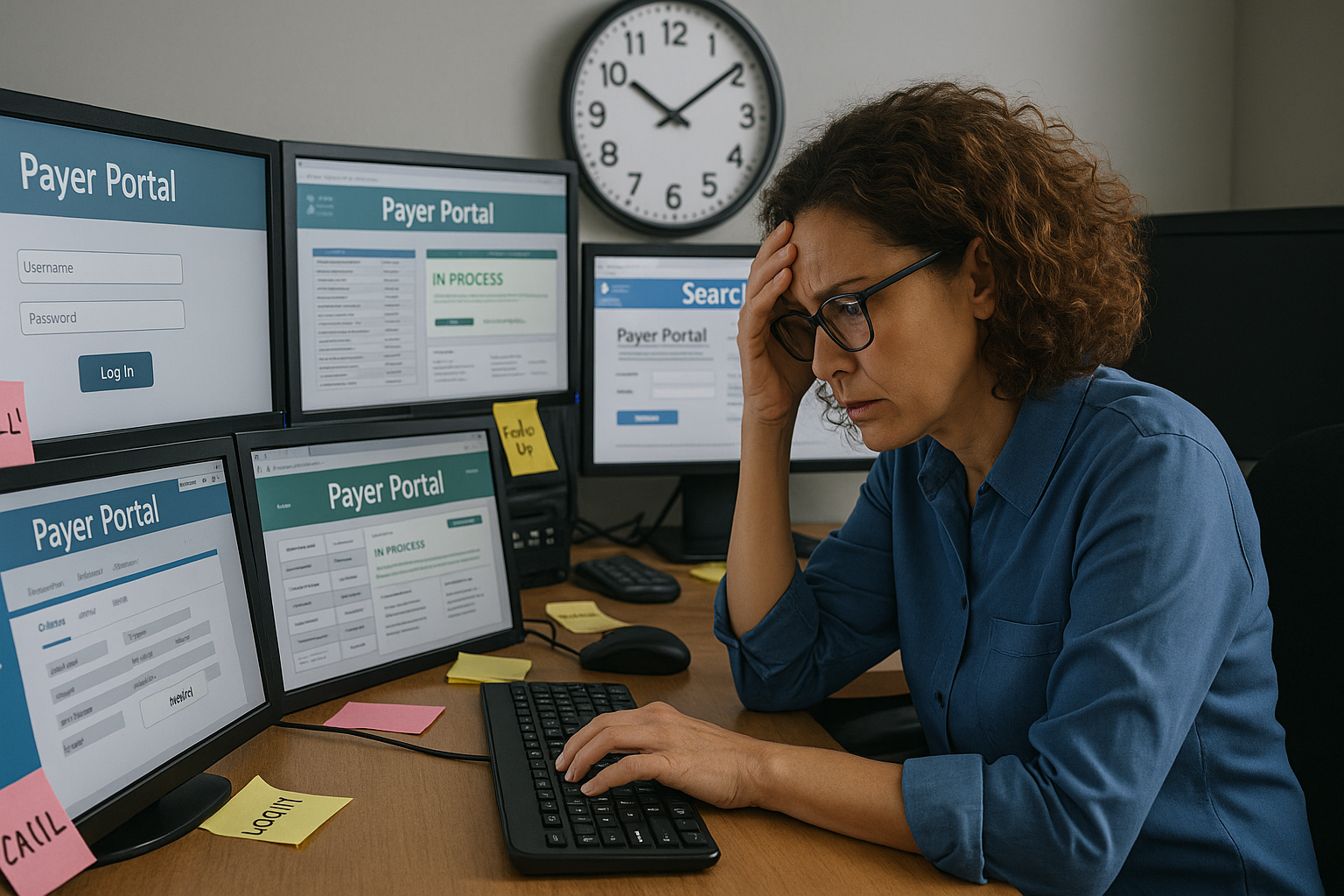
Payers promise transparency and efficiency through their online portals, APIs, and dashboards—but the reality for billing teams is often the opposite. Rather than streamlining workflows, the proliferation of payer-specific tools creates friction, data silos, and duplicated effort. The result? Portal paralysis—when your team is logging into dozens of systems a day, but still not getting…
-
Beyond the Write-Off: How to Prevent Avoidable Patient Bad Debt
It’s easy to chalk up patient balances to bad debt and move on—but doing so quietly drains long-term revenue and damages patient trust. The real issue isn’t patients refusing to pay; it’s the systemic breakdowns in communication, timing, and expectation-setting that make payment unlikely from the start. As high-deductible plans continue to rise and patients…
-
The Credentialing Trap: How Delays at the Start Cripple Your Revenue Cycle

Credentialing is often treated as a standalone task—an administrative checklist that simply needs to be completed before a provider can see patients. But this mindset underestimates the far-reaching consequences of getting it wrong. When credentialing delays occur, the impact ripples downstream: denied claims, unbilled visits, and mounting frustration for patients and staff alike. More Than…
-
The Hidden Revenue Killers in Your RCM Workflow—and How to Fix Them
Are silent revenue leaks sabotaging your revenue cycle performance?If your denial rates are creeping up, AR days are dragging on, or payer audits are catching you off guard—you’re not alone. Despite robust billing systems and EHR integrations, many healthcare organizations still face systemic RCM breakdowns that aren’t easily detected by standard metrics. The good news?…
-
Front Desk Staff: Your Secret Weapon Against Claim Denials (2025 Edition)

How to Transform Patient Access Teams Into Your First Line of Defense The $87,000 Front Desk Mistake “A busy orthopedic clinic lost $87,000 in one quarter because front desk staff weren’t verifying Medicare Advantage plan changes at check-in. Every single claim was denied for eligibility – and all were preventable.” Your front desk staff handle…
