Latest posts
-
Too Many Hands: When Fragmented Billing Ownership Slows Down Reimbursement
Billing isn’t a single task—it’s a process with dozens of interdependent steps. But when too many people are responsible for too many pieces of that process, things start to slip. Claims get stuck in handoffs, accountability gets diluted, and cash flow suffers. If your team is constantly saying, “I thought someone else did that,” it’s…
-
Escalation Fatigue: Why Your AR Team Can’t Get Through to Payers Anymore
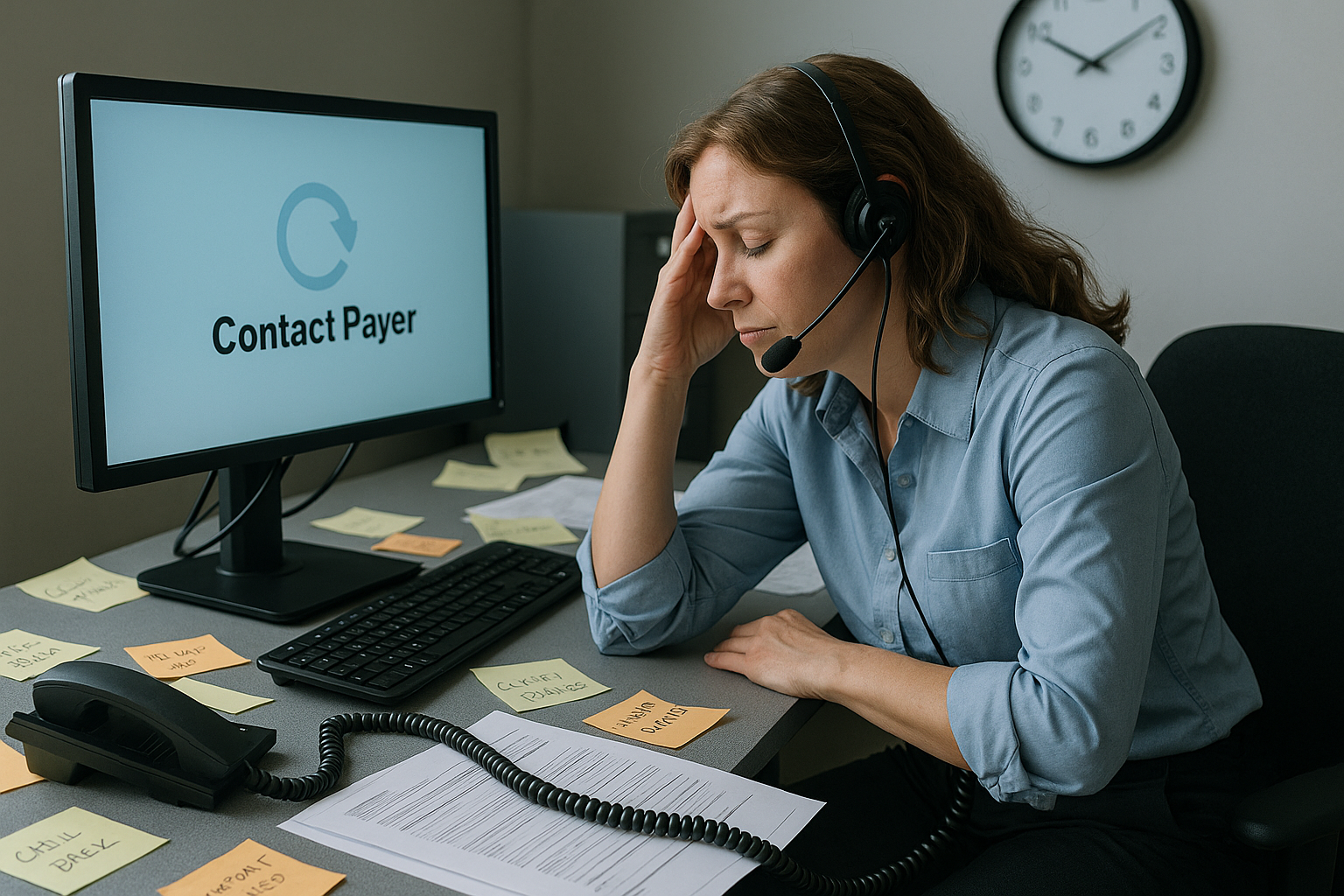
If your AR team spends more time on hold than resolving issues—or if they’re constantly being transferred, disconnected, or “call back later-ed”—you’re not alone. Payers have made it increasingly difficult to escalate inquiries, resolve claim holds, or even speak to a human. The result? Escalation fatigue: a costly blend of burnout, delays, and avoidable write-offs.…
-
🏔️ Authorization Avalanche: Reducing Workflow Bottlenecks in Prior Authorization

The Prior Auth Problem Isn’t Going Away If you feel like getting a prior authorization approved takes longer than delivering care—you’re not alone. Payers are expanding PA requirements across diagnostics, radiology, physical therapy, surgical consults, and even standard medications. As a result: And most dangerously? Claims get denied when PAs aren’t filed—or not filed fast…
-
⏳ Silent Denials: When Payers Don’t Respond and A/R Explodes
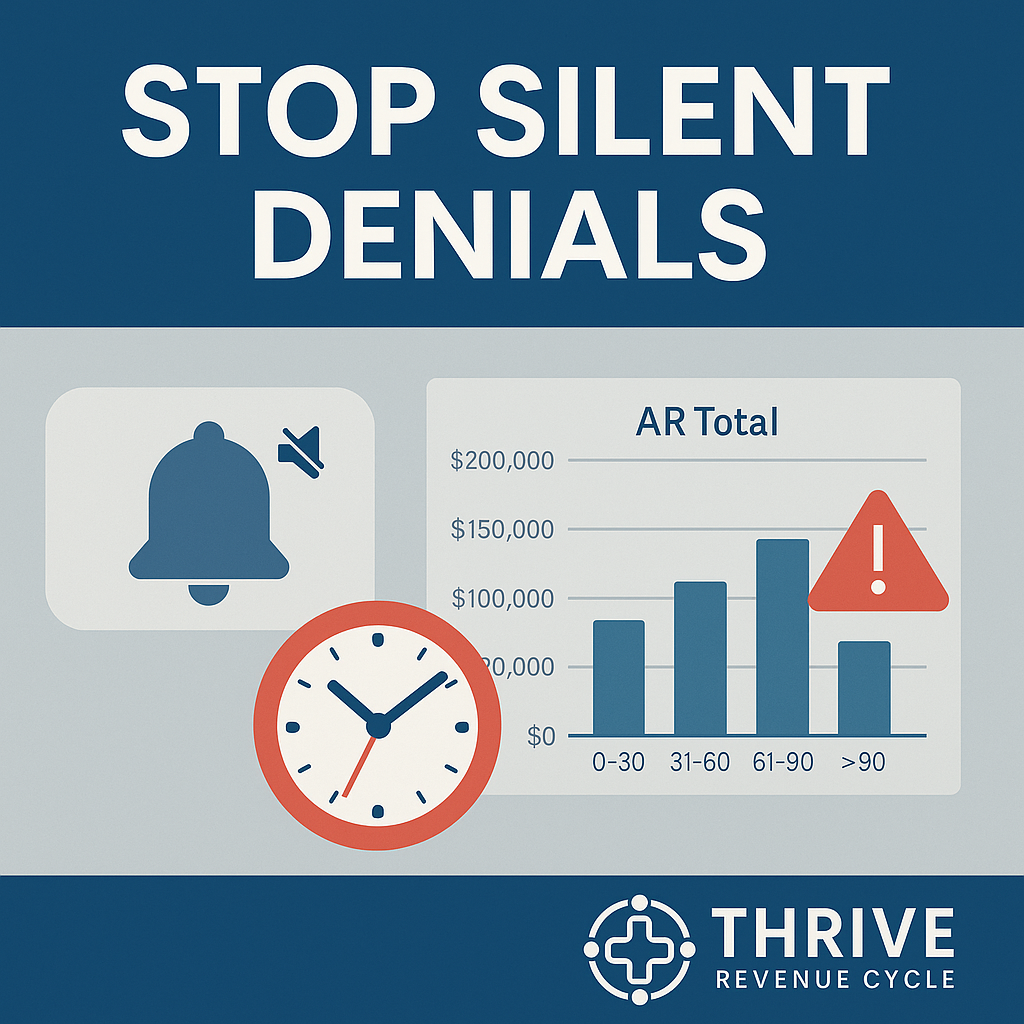
What Are Silent Denials? Unlike formal denials that generate an Explanation of Benefits (EOB) or denial code, silent denials happen when payers simply don’t respond.The claim isn’t processed, isn’t rejected, and isn’t marked as pending. It just… sits there. Why? Silent denials are dangerous because they: The True Cost of Non-Response Every week that a…
-
When Clean Claims Go Dirty: The Hidden Errors Sabotaging Your Reimbursements

The Day the Cash Flow Slowed to a Crawl Last summer, Maria, the practice manager of a busy rural cardiology clinic, was feeling confident. The team had just hit a 94% clean-claim submission rate—a figure that meant faster payments and fewer headaches. But by October, things had changed. Reimbursement timelines were stretching, denials were piling…
-
The $500,000 Lesson: Why Every Revenue Cycle Team Must Document Like Lawyers

How Clear Notes in EHRs Save Revenue, Reduce Call Volume, and Win Appeal “A hospital lost $497,000 because a front desk note simply said ‘insurance verified’ instead of including the verification number. The judge called it ‘insufficient evidence’ – and that’s becoming the rule, not the exception.”* Why Your EHR Notes Are Now Legal &…
-
The Top 5 AI Trends Transforming Healthcare Revenue Cycle Management in 2025

AI is no longer coming for the revenue cycle—it’s already here.From automated eligibility verification to predictive denials and real-time audit readiness, artificial intelligence is rapidly transforming how providers manage the business of healthcare. And while AI holds the potential to eliminate friction and accelerate cash flow, poor implementation—or failure to adapt—can introduce just as many…
