Real-World Revenue Cycle Conversations. No Hype. Just Help.
Healthcare revenue isn’t just about billing codes and payer rules—it’s about people, process, and precision. The Thrive RCM Insider™ explores the operational blind spots, workflow friction, and compliance traps that lead to missed revenue—and offers grounded insights to help you close the gaps.
Whether you’re a clinic manager, billing lead, or compliance officer, you’ll find topics that speak to the real challenges of today’s revenue cycle—written by those who live it.
What You’ll Find Here:
- 🎯 Evidence-backed strategies you can apply today
- 🧠 Smart breakdowns of common pitfalls and policy shifts
- 🛠️ Subtle connections to tools that help—but only where it makes sense
These aren’t fluff pieces or disguised product ads. They’re sharp, honest, and practical resources designed to support your daily decisions—no strings attached.
🚨 Recent Insights
-
🧾 The Front Desk Revenue Drain: How Inaccurate Data Entry Wrecks Clean Claims
First Impressions Matter—To Payers, Too The front desk is your patient’s first touchpoint—but it’s also where many revenue leaks begin. A misspelled name.An outdated insurance ID.A missing referral or authorization. These may seem like small clerical mistakes—but they cause big problems downstream. In fact, up to 80% of denied or rejected claims can be traced […]
-
Too Many Hands: When Fragmented Billing Ownership Slows Down Reimbursement
Billing isn’t a single task—it’s a process with dozens of interdependent steps. But when too many people are responsible for too many pieces of that process, things start to slip. Claims get stuck in handoffs, accountability gets diluted, and cash flow suffers. If your team is constantly saying, “I thought someone else did that,” it’s […]
-
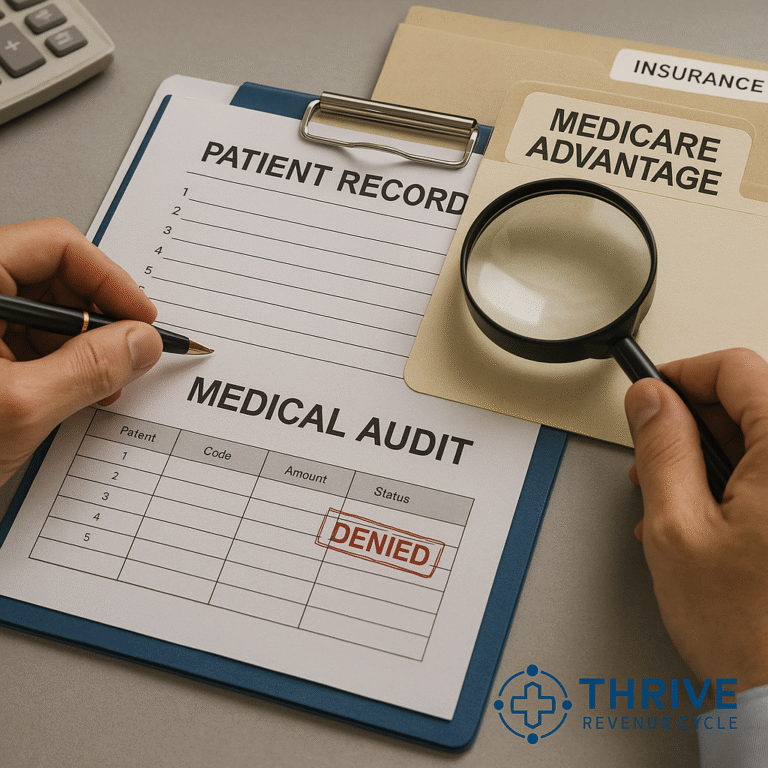
🛡️ Audit-Proofing Your Practice: Preparing for the Rise in Payer Retrospective Reviews
Retrospective Audits Are on the Rise In the past, most payer audits focused on prepayment reviews or prior authorization compliance. But not anymore. Retrospective audits—where payers request documentation months or even years after payment—are rapidly increasing.And they’re not just looking for errors—they’re looking for money to claw back. Why the increase? The Hidden Cost of […]
-
Escalation Fatigue: Why Your AR Team Can’t Get Through to Payers Anymore
If your AR team spends more time on hold than resolving issues—or if they’re constantly being transferred, disconnected, or “call back later-ed”—you’re not alone. Payers have made it increasingly difficult to escalate inquiries, resolve claim holds, or even speak to a human. The result? Escalation fatigue: a costly blend of burnout, delays, and avoidable write-offs. […]
-
⚖️ The Compliance Lag: Why Billing Teams Struggle to Keep Pace with Regulatory Changes
Why Staying Current Feels Impossible Keeping up with payer policies and government regulations used to be a quarterly task.Now, it’s a weekly scramble. From CMS’s 2025 Final Rule to mid-year commercial payer policy edits, the volume and velocity of change in healthcare billing is staggering. What’s making this harder: The result?Claims get denied, money gets […]
-
Under the Radar: How Small Denials Add Up to Big Losses
It’s easy to focus your team’s energy on the big-ticket denials—high-dollar claims that demand attention. But while those denials are obvious, what’s often overlooked are the low-dollar, low-effort denials that quietly accumulate and slowly drain your revenue. The $15 here, the $42 there—they may seem insignificant in isolation, but across a month or quarter, these […]
📚 Thrive Knowledge Hub
Explore Deeper. Learn Smarter.
Not every revenue challenge can be solved in a headline—and that’s where our archive comes in. The Thrive RCM Archives™ are a curated library of previous posts packed with real-world insights, expert commentary, and actionable strategies across the revenue cycle.
We feature the latest six articles on the Thrive RCM Insider homepage to spotlight fresh thinking. But when you’re digging into persistent pain points, or training your team, the archives offer a deeper well of knowledge to draw from.
🧠 What You’ll Find:
- Trends in payer behavior, denial patterns, and regulatory shifts
- Workflow tips and optimization ideas from RCM pros
- Long-form breakdowns of tough operational blind spots
✅ How to Use the Archives:
- Skim or Study – Use articles as quick refreshers or deeper guides in team huddles or staff meetings.
- Explore Patterns – See how past issues (like AR delays or audit risks) evolved—and how others have tackled them.
- Cross-Reference – Many articles point to practical tools and frameworks—use them as a springboard, not a sales pitch.
💬 “We want these articles to earn a place in your bookmark bar—not your spam folder. If it’s not useful, it’s not published.”