Fight Smarter. Reverse Faster. Stop Letting Revenue Slip Away.
Appeals don’t have to be a scramble. Whether you’re drowning in preventable denials, juggling outdated letter templates, or struggling to track what’s been appealed — this suite gives you the tactical edge to reclaim what’s rightfully yours.
🛠 This collection includes:
🛡️ The Appeal Shield™ – Pre-written appeal letters, payer packs, and specialty templates
🛡️ Appeal Shield™ – Tracker Guard™ – Denial tracker tools and appeal monitoring templates
🛡️ Review Shield™ – Denial diagnostics, claim audits, and optimization roadmaps
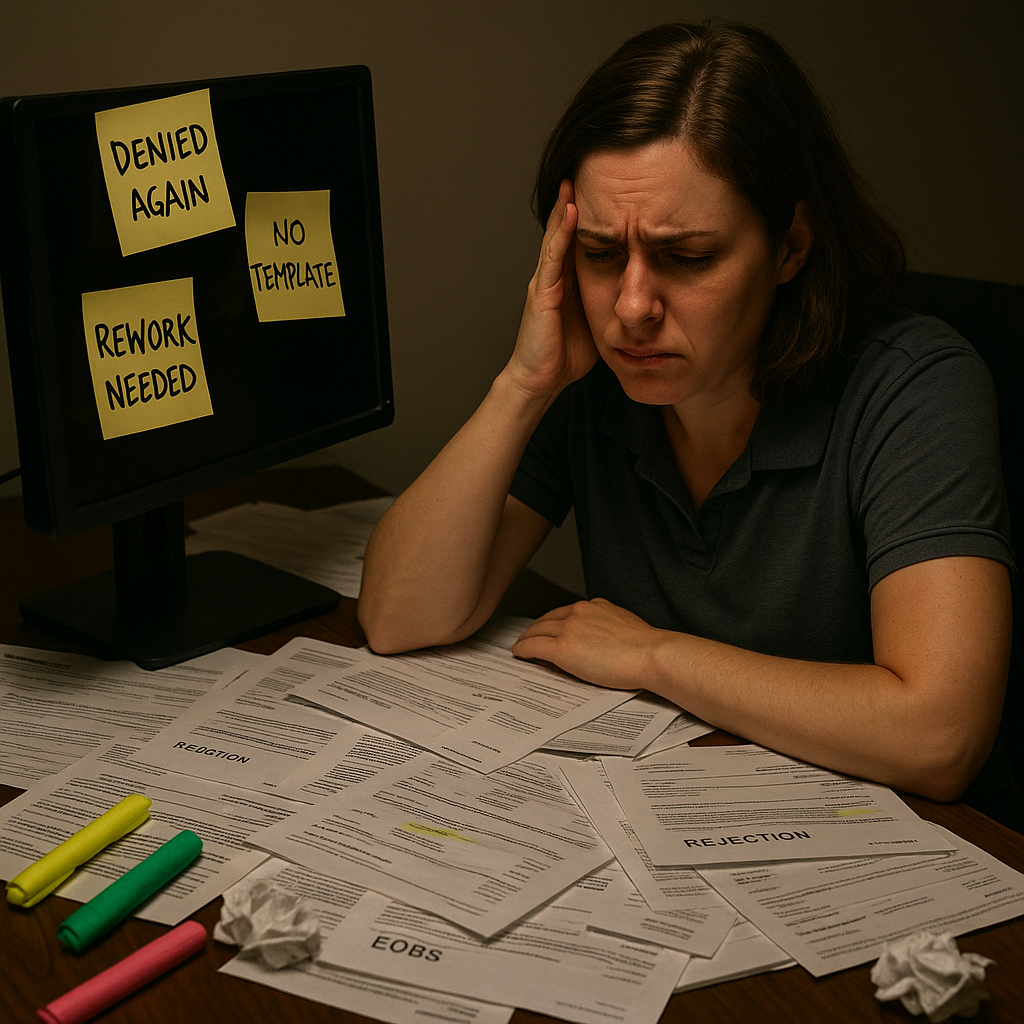
❗ The Denial Dilemma
Even the best-run clinics still struggle with:
🚫 The same denials repeated month after month
🧱 No standard appeal process or policy
📤 Staff re-writing appeals from scratch
📉 Denials tracked on outdated spreadsheets
🤯 Unclear denial root causes and poor prevention
⏳ Delayed appeals leading to permanent write-offs
It’s not just annoying. It’s expensive.
⚡ Who This Is For
✅ Denial Follow-Up Teams buried in appeals and rewrites
✅ RCM Managers who want to reduce write-offs and backlog
✅ Billing Leads tired of copy/paste appeal chaos
✅ New Staff who need plug-and-play scripts
✅ Owners trying to uncover and stop revenue leaks
💸 The Cost of Not Acting
You could be losing $25K+ per month just from write-offs and preventable denials.
Not to mention:
- Unrecovered revenue due to missed appeal deadlines
- Increased compliance risk from inconsistent appeal practices
- Lower team morale and higher staff burnout
- Longer days for your already stretched billing team
💡 Choose the Right Tool for Your Denial Pain Point
Each tool is fully standalone — choose based on where your appeal process breaks down.
🛡️ The Appeal Shield™
Stop Starting From Scratch. Win Back Denials With Confidence.
This toolkit gives your team a head start — pre-written appeal letters, organized by denial type, payer, and specialty. Skip the guesswork and start reversing revenue loss faster.
📦 Five Tiers Available:
| Tier | Price | Description |
|---|---|---|
| Core Set | $349 | Includes 25 common denial appeal templates with plug-and-play citations |
| Payer Packs | $599 | Includes 60 letters referencing payer-specific rules (UHC, Aetna, etc.) |
| Facility Packs | $599 | Includes 75 letters citing federal billing regulations (CAH, RHC, FQHC) |
| Custom Clinic Set | $749 | Tailored 1:1 to your common denials, specialties, and state |
| Denial Master Bundle | $1,495 | All-in-one package with every template and format included |
🧰 Includes: Word + Portal formats, citations, denial reason indexes, and customization guidance
👉 Explore The Appeal Shield™ →
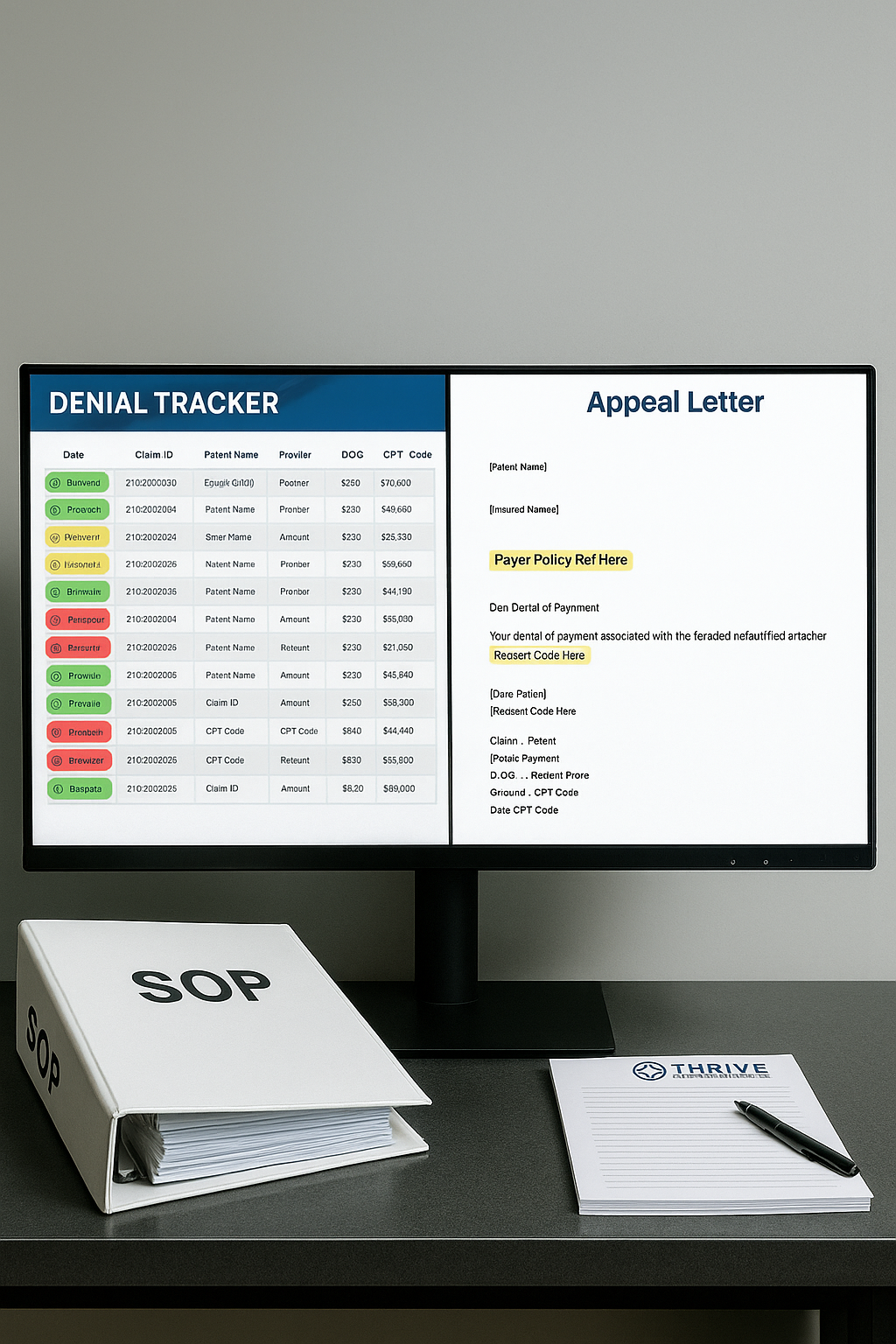
🛡️ Appeal Shield™ – Tracker Guard™
Finally, a Denial Tracker Built for Real Clinics.
Track, sort, and resolve denials with clarity. This plug-and-play tracker is designed for teams without expensive denial management software — and it works.
📦 Two Tiers Available:
| Tier | Price | Description |
|---|---|---|
| Self-Setup | $299 | Includes Excel/Sheets-based denial tracker, sample dashboards, and logging fields |
| Guided Setup | $495 | Adds setup walkthrough, customization help, and staff usage checklist |
🧰 Includes: Status tracking, payer filtering, appeals calendar, team assignments
🛡️ Review Shield™
Don’t Guess — Diagnose What’s Really Causing Denials.
Perfect for practices looking to improve workflows, spot billing gaps, or prep for a denial cleanup sprint.
📦 Three Tiers Available:
| Tier | Price | Description |
|---|---|---|
| Lite Diagnostic | $695 | Includes denial pattern analysis, sample audits, and risk scoring |
| Standard Review | $1,250 | Adds claims sampling, team recommendations, and 30-day remediation roadmap |
| Premium Optimization | $2,000 | Includes full-cycle analysis, provider training insights, and documentation coaching |
🧰 Includes: Claim audit templates, payer review forms, clinical denial patterns
🧠 Results You Can Expect
✔ Faster, more successful appeals
✔ Staff who feel confident fighting denials
✔ Timely tracking and recovery of revenue
✔ Reduced write-offs from avoidable errors
✔ Stronger payer response with evidence-based citations

“We recovered $40,000 in denied claims within 60 days using Appeal Shield™.”
Kelsey R.
RCM Manager
📦 Product Summary
| Product | Tiers | Starting At |
|---|---|---|
| 🛡️ The Appeal Shield™ | 5 Tiers | $349 |
| 🛡️ Appeal Shield™ – Tracker Guard™ | 2 Tiers | $299 |
| 🛡️ Review Shield™ | 3 Tiers | $695 |
