Protect Virtual Revenue. Stay Audit-Ready.
A targeted compliance audit and correction system built for telehealth billing—designed to eliminate denials, prevent recoupments, and align your claims with constantly evolving payer rules.
📋 Includes modifier/POS audits, documentation review, and payer-specific telehealth rules across Medicare, Medicaid, and commercial plans.
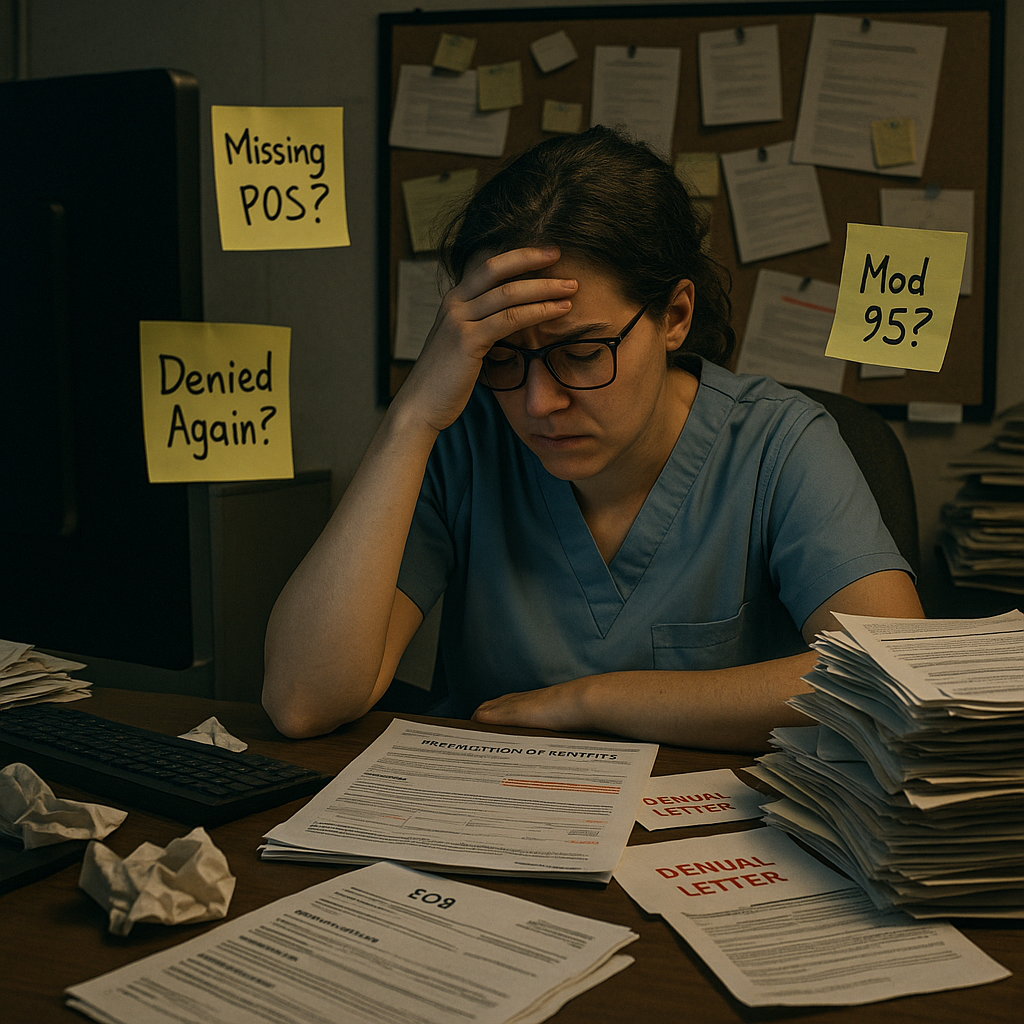
❗ The Problem with Telehealth Billing
Even experienced billing teams struggle with the fast-changing rules around virtual care. Mistakes lead to denials, lost revenue, or post-payment audits—and most teams don’t even realize they’re noncompliant until it’s too late.
🚨 Common Risk Triggers
- Incorrect use of modifier 95, GT, or GQ across CPTs
- POS errors tied to payer-specific rules
- Documentation gaps that don’t support billed services
- Conflicting guidelines between Medicare, Medicaid, and Commercial payers
- Lack of standardized SOPs or staff training
Every missed rule = a denial, recoupment, or compliance finding.
✅ Who It’s For
🛡 What’s Inside The Telehealth Shield™
🎯 A complete compliance toolkit to validate and improve your virtual care billing process.
| Feature | Description |
|---|---|
| 📋 Telehealth Claims Audit | Audit of sample-size or full claim set (based on plan) |
| 🧾 Modifier & POS Review | Payer-aligned checks for CPT + modifier + POS combinations |
| 📂 Documentation Review | Spot gaps in provider notes, CPT support, and timing |
| 🛠 Corrective Action Plan | Clear remediation roadmap with timelines |
| 🧠 Team Training Session | Optional coaching for coders and billing staff |
| 📚 Payer Rule Crosswalk | Up-to-date side-by-side Medicare, Medicaid, Commercial policy grid |
| 🧩 Optional Add-Ons | Appeal letters, SOP kits, and doc-to-code visual guides |
🧰 Plan Comparison & Pricing
A pricing table assists users in selecting a suitable plan by simply and clearly differentiating product/service features and prices. Use this as supporting text for your plans.
Audit of 25 claims, modifier/POS check, red flag summary
Spot the red flags before payers do.
🛡️ Full Review
Audit of 100 claims, full action plan, staff training session
Build your plan. Train your team. Protect every claim.
Add-On Menu
Expand support with SOPs or appeals
SOPs for billing workflows, POS logic, and EHR templates
Standardize your telehealth workflow in one plug-and-play kit.
📤 Appeal Letter Pack – Telehealth Edition
10 payer-aligned appeal templates for denied virtual claims
Get 10 prewritten appeals that speak your payers’ language.
Visual guides to improve provider documentation and billing support
Let your user know what to expect when choosing this plan. Inform users of plan benefits, not features.
📈 Results You Can Expect
✔ Fewer denials and faster resolution of virtual claims
✔ Clean modifier and POS alignment with payer policies
✔ Stronger documentation support in EHR and provider notes
✔ Trained, confident staff that can prevent future errors
✔ Clear audit trail to withstand payer reviews or pre-pay edits

🗨️ “We thought we were coding correctly—until the audit revealed our POS use was wrong across 2 payers. This saved us thousands.”
Jenna R.
Billing Manager
