Protect Your Compliance. Recover Revenue. Simplify Operations.
Tailored audit support and denial management strategies for
RHCs, CAHs, and FQHCs—built to match the specific federal rules, billing models, and clinical operations of your facility type.
📋 Each plan includes:
- Facility-specific denial appeal templates
- Audit-proof SOPs and compliance workflows
- Strategic walkthroughs to ensure team readiness
✅ Stay compliant.
💸 Get paid what you’ve earned.
📉 Minimize audit and denial risk.
👉 Choose your facility type below to get started.
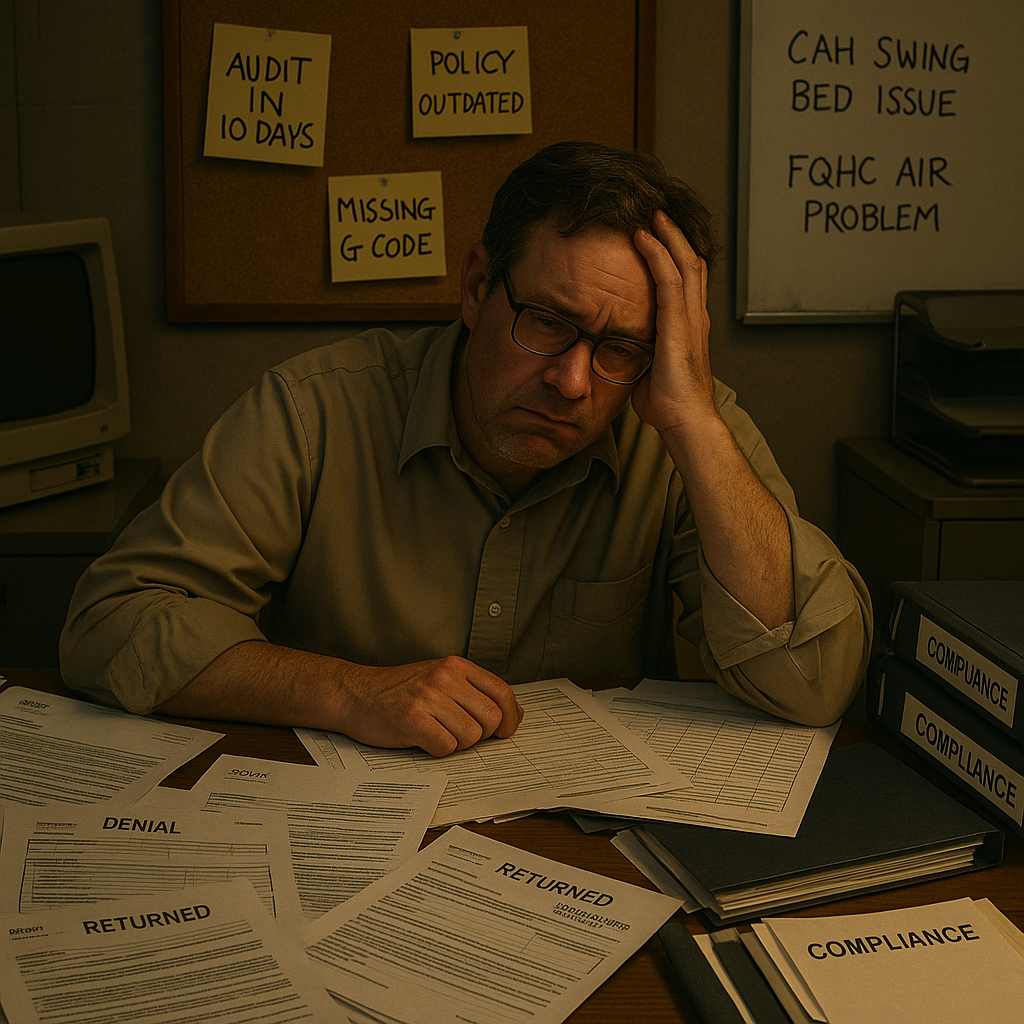
❗ The Challenge for Federally Designated Clinics
RHCs, CAHs, and FQHCs operate at the intersection of mission and regulation. You’re serving vulnerable communities—but your ability to stay open depends on navigating complex billing rules, denial patterns, and compliance audits.
- 🧾 Confusing Payment Models
Whether you bill under cost-based reimbursement (RHCs, CAHs), PPS (FQHCs), or hybrid arrangements—errors in claim setup, modifier usage, or encounter coding lead to underpayments and clawbacks. - 💥 High Denials with Limited Support
Your designation adds extra scrutiny from MACs, MCOs, and commercial payers—but off-the-shelf denial tools don’t reflect your federal carve-outs or state-level exceptions. - 👥 Understaffed. Overloaded. Undersupported.
Your billing team wears multiple hats. You don’t need theory—you need targeted strategy that meets you where you are: your EHR, your workflows, your staffing limits.
✅ When to Choose Rural Shield™
- You need facility-type-specific tools that reflect your actual billing model
- You’ve had payer audit requests or patterned denials (CO97, CO16, CO45, etc.)
- You want ready-to-send appeal templates with citations to federal regulations
- You’re preparing for an audit and need SOPs or logs to show due diligence
- Your team needs a clearer roadmap for reducing risk and recovering revenue
💸 The Cost of Not Acting
- Denials sit unresolved while deadlines pass
- Audit requests arrive with no clear owner or strategy
- Staff rely on Google or outdated PDFs for complex billing issues
- Failed audits create CAPs, repayment, or reputational damage
- Compliance lives in the heads of a few people—and they’re overwhelmed
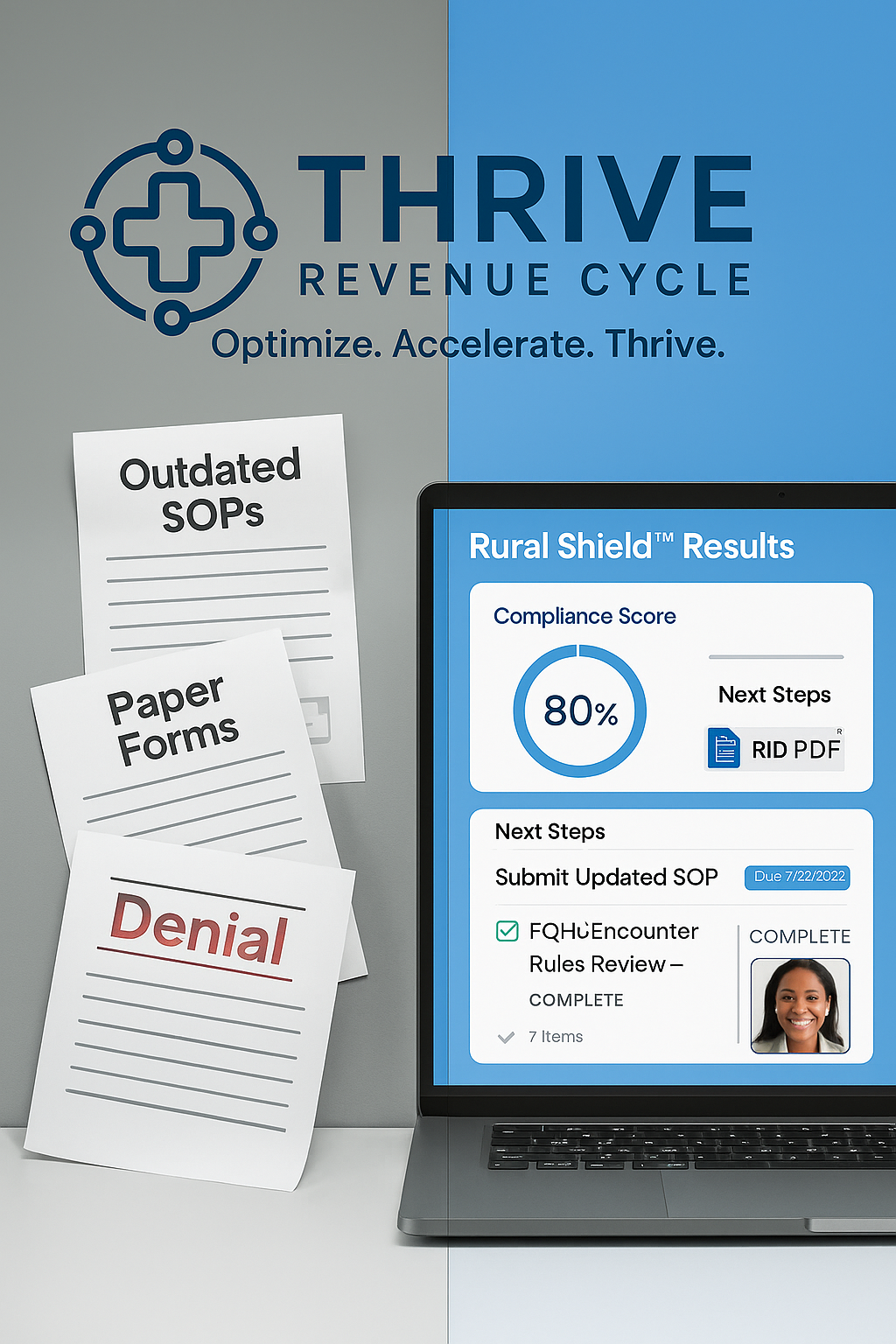
🛡️ Meet Rural Shield™
Rural Shield™ is a facility-type-specific compliance and denial toolkit for clinics serving rural and underserved communities. It includes everything your team needs to prepare for audits, reverse denials, and stay aligned with the regulations that govern your specific clinic model.
🎯 How It Helps
✔ Provides facility-specific denial templates with policy citations
✔ Includes audit-ready SOPs, logs, and checklists
✔ Breaks down what applies to RHCs, CAHs, and FQHCs—with clarity
✔ Helps non-compliance team members contribute confidently
✔ Improves documentation, tracking, and escalation workflows
✔ Gives your team the tools to act fast when denials or audits hit
💼 What’s Included
Each Rural Shield™ pack includes clinic-type-specific tools:
✅ Denial Appeal Letter Templates – With citations to CMS, MACs, or HRSA policies
✅ Audit Preparation Checklists – For internal tracking and CAP response
✅ Facility-Specific SOPs – Tailored to billing flow, visit types, and compliance risks
✅ Denial Log Templates – Track, trend, and assign denial follow-up
✅ Submission Timelines + Policy Links – For common payers (Medicare, Medicaid, Commercial)
✅ Training Aids – Tools for internal compliance education or team refreshers
✅ Editable Formats – Word, Excel, and PDF files for easy customization
✅ What You’ll Get with The Rural Shield™
- A facility-type-specific strategy track (RHC, CAH, or FQHC)
- A custom roadmap to fix your biggest audit, documentation, or billing risks
- Three plug-and-play compliance tools tailored to your setting
- Optional denial letters or SOP bundles to complete your toolkit
Rural Health Clinics (RHCs)
You’ll Receive:
- RHC Modifier Quick Guide™
- Visit Type SOP Snapshot™
- Cost Reconciliation Readiness Checklist™
“This gave us a real understanding of how to clean up our UB-04 billing and prevent errors that trigger MAC reviews.”
— Deb C., RHC Manager, Iowa
Critical Access Hospitals (CAHs)
You’ll Receive:
- CAH Revenue Mapping Tool™
- CAH UB-04 Billing SOP Snapshot™
- Modifier & Bundling Map™
“We uncovered denial trends linked to our therapy and ED departments that we never tracked before.”
— Nathan S., CAH Billing Supervisor, Wyoming
Federally Qualified Health Centers (FQHCs)
You’ll Receive:
- FQHC Visit Type Coding Guide™
- PPS Payment Review Tool™
- Sliding Fee SOP Template™
“HRSA and PPS compliance used to overwhelm us—this broke it down into actionable tools for our front desk and billing team.”
— Latasha R., FQHC Director, Georgia
Protect Your Compliance. Recover Revenue. Simplify Operations.
Each pack includes tailored denial templates, SOPs, logs, checklists, and compliance trackers to help your clinic reduce audit risk, reverse denials faster, and confidently meet CMS expectations.
60-min consult + roadmap + 1 compliance tool
Get a Clear Pulse Check Before Problems Grow.
🛡️ Full Engagement
Full audit + roadmap + 3 tailored tools
Fix What’s Broken. Fortify What Works
Expand support with denial templates or SOP kits
Facility-specific SOPs for modifiers, visits, billing
Start with SOPs That Make Sense.
📤 Appeal Letter Pack
10 templates aligned with your clinic’s billing logic
Send Appeals That Actually Win.
📈 Results You Can Expect
✔ Stronger audit prep with fewer last-minute scrambles
✔ Faster reversal of common denials like CO16, CO97, CO45, CO18
✔ Confidence knowing your SOPs, logs, and trackers match federal rules
✔ Empowered staff who understand what applies to your clinic
✔ Peace of mind when surveyors, MACs, or payers come calling

