When Copy-Paste Appeals Stop Working
Two months ago, Jason, the revenue cycle director at a mid‑sized orthopedic practice, noticed a troubling trend. His team was sending appeal letters for denied claims faster than ever, using the same “tried‑and‑true” templates they’d relied on for years. But payer overturn rates were slipping—from 68% to just 41%. The team’s productivity was high, but their results told another story: the templates weren’t keeping up with payer tactics, and they were unknowingly fighting the same battles over and over.
Why Generic Appeals Fail
On the surface, appeal templates seem like a time saver. They let staff respond quickly, ensure a professional tone, and cover the basics. But here’s the problem:
- Payers are adapting. They spot mass‑produced letters and respond with boilerplate denials.
- The root cause isn’t addressed. A letter alone doesn’t fix coding errors, documentation gaps, or missing prior authorizations that triggered the denial in the first place.
- Evidence is missing. Without payer‑specific citations or claim‑level documentation, even a well‑written letter is easy to dismiss.
In Jason’s case, many denials were caused by the same eligibility verification errors that had never been corrected. The appeal letters only addressed the symptom—not the source.
The Root of the Problem: Lack of Denial Intelligence
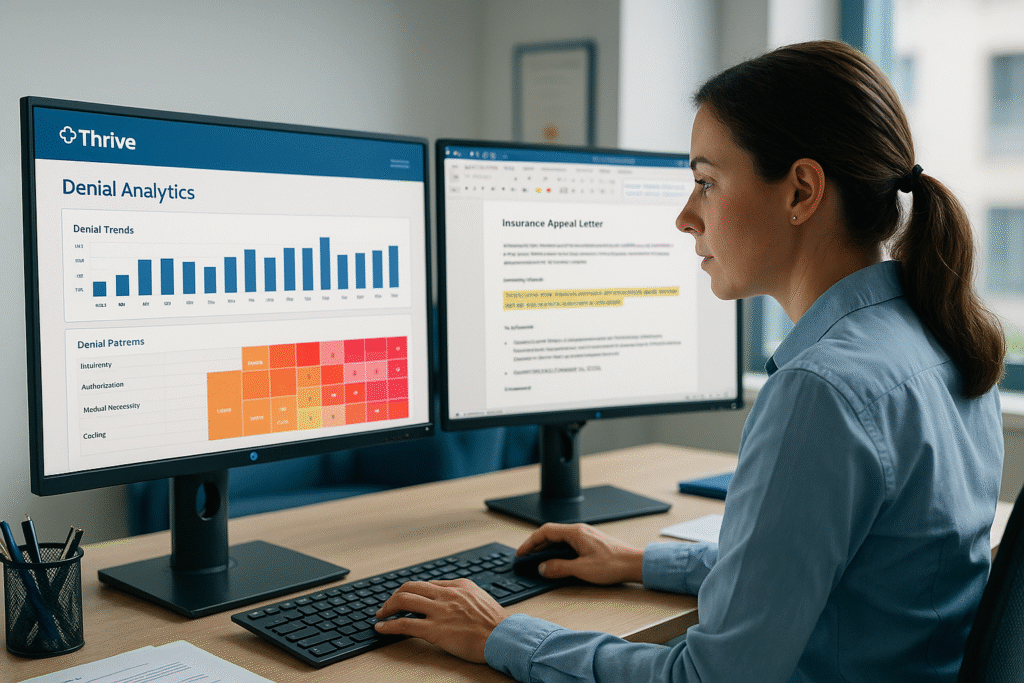
Appeals fall short when teams lack denial analytics that pinpoint patterns. Without visibility into denial codes, payer rules, and recurring process breakdowns, staff are working in the dark.
Three common intelligence gaps that hurt appeal success:
- No denial pattern analysis – Teams can’t see the high‑volume denial types most worth targeting.
- Missing payer policy references – Letters lack the citations that carry weight in overturn decisions.
- Disconnected workflows – Denial prevention steps aren’t fed back into front‑end processes, so errors repeat.
How to Build Appeals That Actually Win
Winning appeals are backed by data, tailored to the payer, and tied to prevention strategies.
Best Practices for High‑Impact Appeals:
- Analyze Denial Trends First – Use a denial pattern heatmap to identify your top codes and payers.
- Integrate Payer Policies – Include direct references to CMS LCD/NCDs or commercial payer manuals.
- Customize Per Case – Adjust tone, evidence, and citations for the specific denial reason.
- Close the Loop – Feed the root cause back into front‑end fixes so you see fewer repeats.
When Jason’s team adopted a data‑driven appeals strategy through denial analytics, they cut repetitive denials by 22% in three months. They still used templates—but as a foundation, not the final word. Each appeal included denial‑specific evidence, payer citations, and proof that the claim met the requirements.
Turning Denials into Recovered Revenue
For Jason’s clinic, the difference was clear: fewer wasted appeals, more overturns, and a visible drop in the denial rate. It wasn’t about sending more letters—it was about sending the right ones, backed by solid intelligence.
If you’re ready to stop fighting denials blind and start winning with precision, explore Denial Shield. It combines denial pattern analytics, payer‑specific appeal strategies, and ready‑to‑customize letter frameworks so your team can turn denials into revenue.