Latest posts
-
⚙️ When AI Misses the Mark: Preventing Automation-Driven Errors in RCM

The Promise and Peril of AI in Revenue Cycle Artificial Intelligence (AI) has moved from buzzword to baseline in healthcare revenue cycle operations. Today, practices use AI for: But here’s the catch: AI only works as well as its rules, data, and oversight. And when those fail? You don’t just lose efficiency—you lose revenue. Common…
-
Beyond the Write-Off: How to Prevent Avoidable Patient Bad Debt
It’s easy to chalk up patient balances to bad debt and move on—but doing so quietly drains long-term revenue and damages patient trust. The real issue isn’t patients refusing to pay; it’s the systemic breakdowns in communication, timing, and expectation-setting that make payment unlikely from the start. As high-deductible plans continue to rise and patients…
-
Appeals That Actually Win: Beyond Templates to Root-Cause Fixes

When Copy-Paste Appeals Stop Working Two months ago, Jason, the revenue cycle director at a mid‑sized orthopedic practice, noticed a troubling trend. His team was sending appeal letters for denied claims faster than ever, using the same “tried‑and‑true” templates they’d relied on for years. But payer overturn rates were slipping—from 68% to just 41%. The…
-
🎯 Chasing the Wrong Denials: How to Prioritize High-Impact Appeals

Not All Denials Are Worth It Let’s be honest: appealing every denial isn’t efficient—it’s exhausting. Too many revenue cycle teams default to working appeals based on when they show up in the queue, not based on strategic value. The result? It’s time to stop treating all denials the same. The Real Cost of Low-Value Appeals…
-
When Clean Claims Go Dirty: The Hidden Errors Sabotaging Your Reimbursements

The Day the Cash Flow Slowed to a Crawl Last summer, Maria, the practice manager of a busy rural cardiology clinic, was feeling confident. The team had just hit a 94% clean-claim submission rate—a figure that meant faster payments and fewer headaches. But by October, things had changed. Reimbursement timelines were stretching, denials were piling…
-
The Credentialing Trap: How Delays at the Start Cripple Your Revenue Cycle

Credentialing is often treated as a standalone task—an administrative checklist that simply needs to be completed before a provider can see patients. But this mindset underestimates the far-reaching consequences of getting it wrong. When credentialing delays occur, the impact ripples downstream: denied claims, unbilled visits, and mounting frustration for patients and staff alike. More Than…
-
📚 Training Fatigue: Why Annual Compliance Training Isn’t Enough

The Problem with the Once-a-Year Approach Let’s face it: most annual compliance training is forgettable.Employees click through generic modules, pass a quiz, and move on—only to forget 80% of what they learned within a few weeks. In high-risk environments like billing, coding, patient access, and clinical documentation, this leads to: Annual training may check the…
-
Lost in the Loop: Why Claim Status Codes Aren’t Giving You the Full Picture
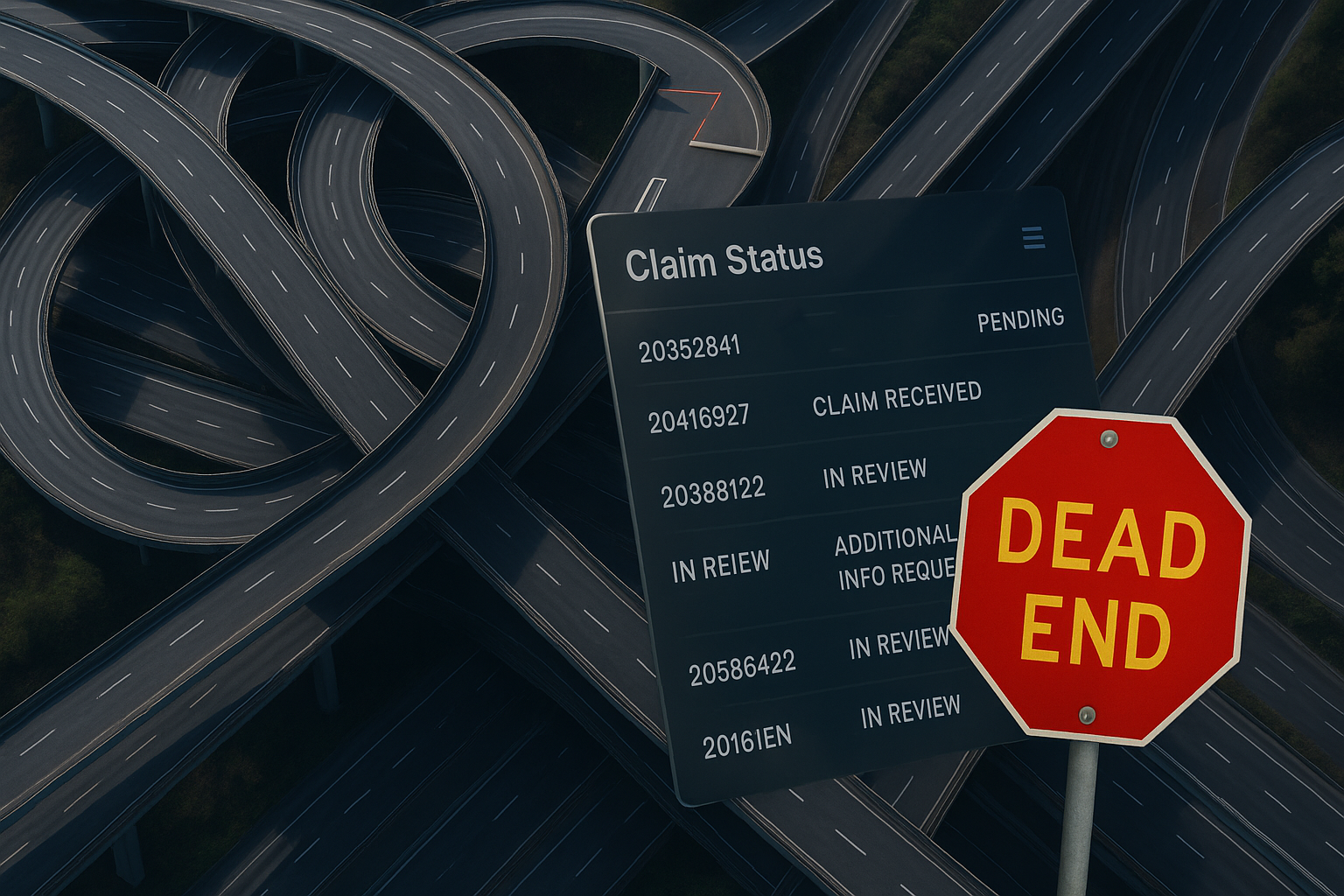
Claim status codes were designed to bring clarity—but for most billing teams, they’ve done the opposite. Instead of delivering transparency, these standardized codes often offer vague or incomplete answers that lead to more questions, longer resolution times, and frustrating payer phone calls. When a claim is stuck in limbo, relying solely on the status code…
