Latest posts
-
🧾 The Front Desk Revenue Drain: How Inaccurate Data Entry Wrecks Clean Claims

First Impressions Matter—To Payers, Too The front desk is your patient’s first touchpoint—but it’s also where many revenue leaks begin. A misspelled name.An outdated insurance ID.A missing referral or authorization. These may seem like small clerical mistakes—but they cause big problems downstream. In fact, up to 80% of denied or rejected claims can be traced…
-
Too Many Hands: When Fragmented Billing Ownership Slows Down Reimbursement
Billing isn’t a single task—it’s a process with dozens of interdependent steps. But when too many people are responsible for too many pieces of that process, things start to slip. Claims get stuck in handoffs, accountability gets diluted, and cash flow suffers. If your team is constantly saying, “I thought someone else did that,” it’s…
-
🛡️ Audit-Proofing Your Practice: Preparing for the Rise in Payer Retrospective Reviews

Retrospective Audits Are on the Rise In the past, most payer audits focused on prepayment reviews or prior authorization compliance. But not anymore. Retrospective audits—where payers request documentation months or even years after payment—are rapidly increasing.And they’re not just looking for errors—they’re looking for money to claw back. Why the increase? The Hidden Cost of…
-
Escalation Fatigue: Why Your AR Team Can’t Get Through to Payers Anymore
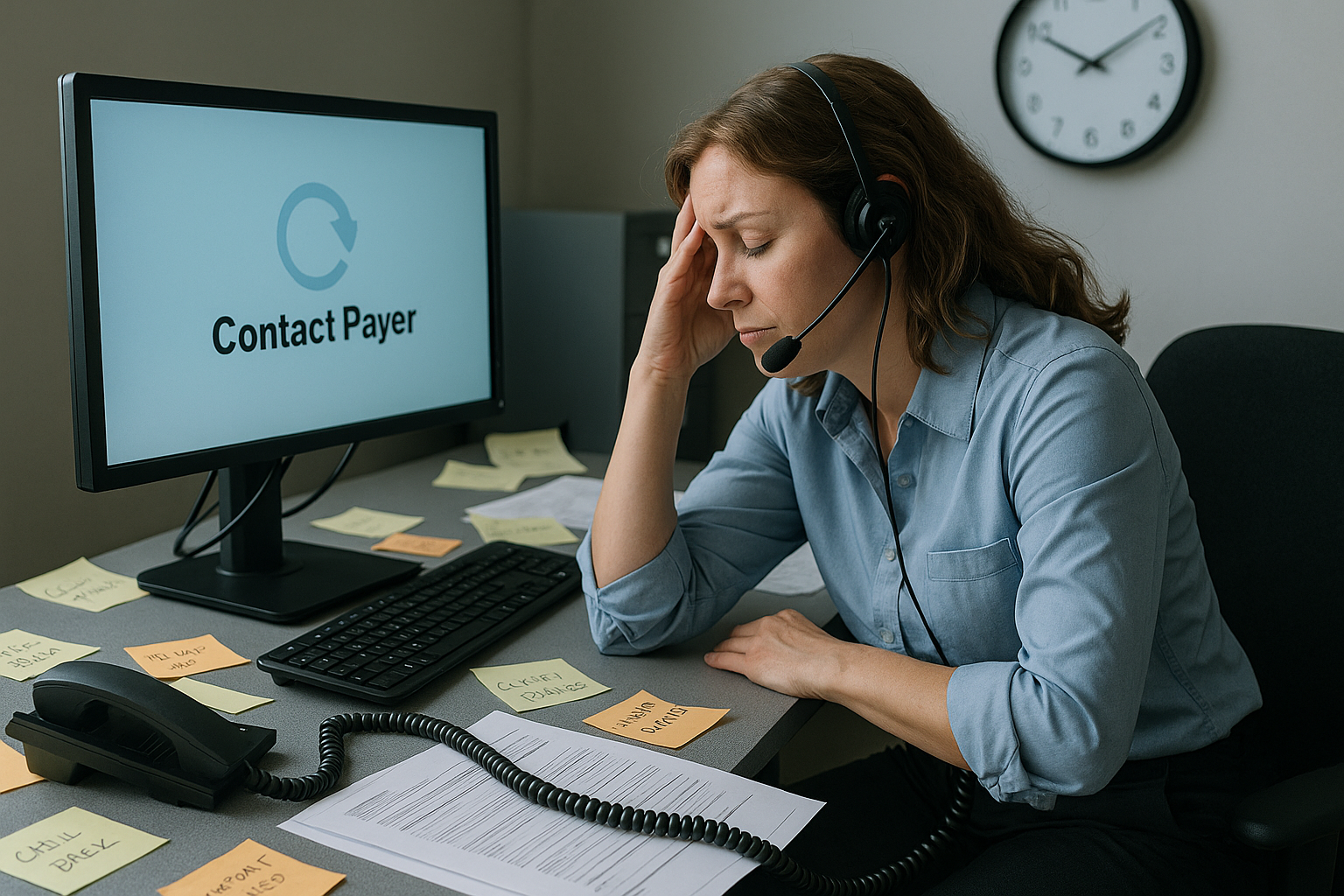
If your AR team spends more time on hold than resolving issues—or if they’re constantly being transferred, disconnected, or “call back later-ed”—you’re not alone. Payers have made it increasingly difficult to escalate inquiries, resolve claim holds, or even speak to a human. The result? Escalation fatigue: a costly blend of burnout, delays, and avoidable write-offs.…
-
⚖️ The Compliance Lag: Why Billing Teams Struggle to Keep Pace with Regulatory Changes

Why Staying Current Feels Impossible Keeping up with payer policies and government regulations used to be a quarterly task.Now, it’s a weekly scramble. From CMS’s 2025 Final Rule to mid-year commercial payer policy edits, the volume and velocity of change in healthcare billing is staggering. What’s making this harder: The result?Claims get denied, money gets…
-
Under the Radar: How Small Denials Add Up to Big Losses
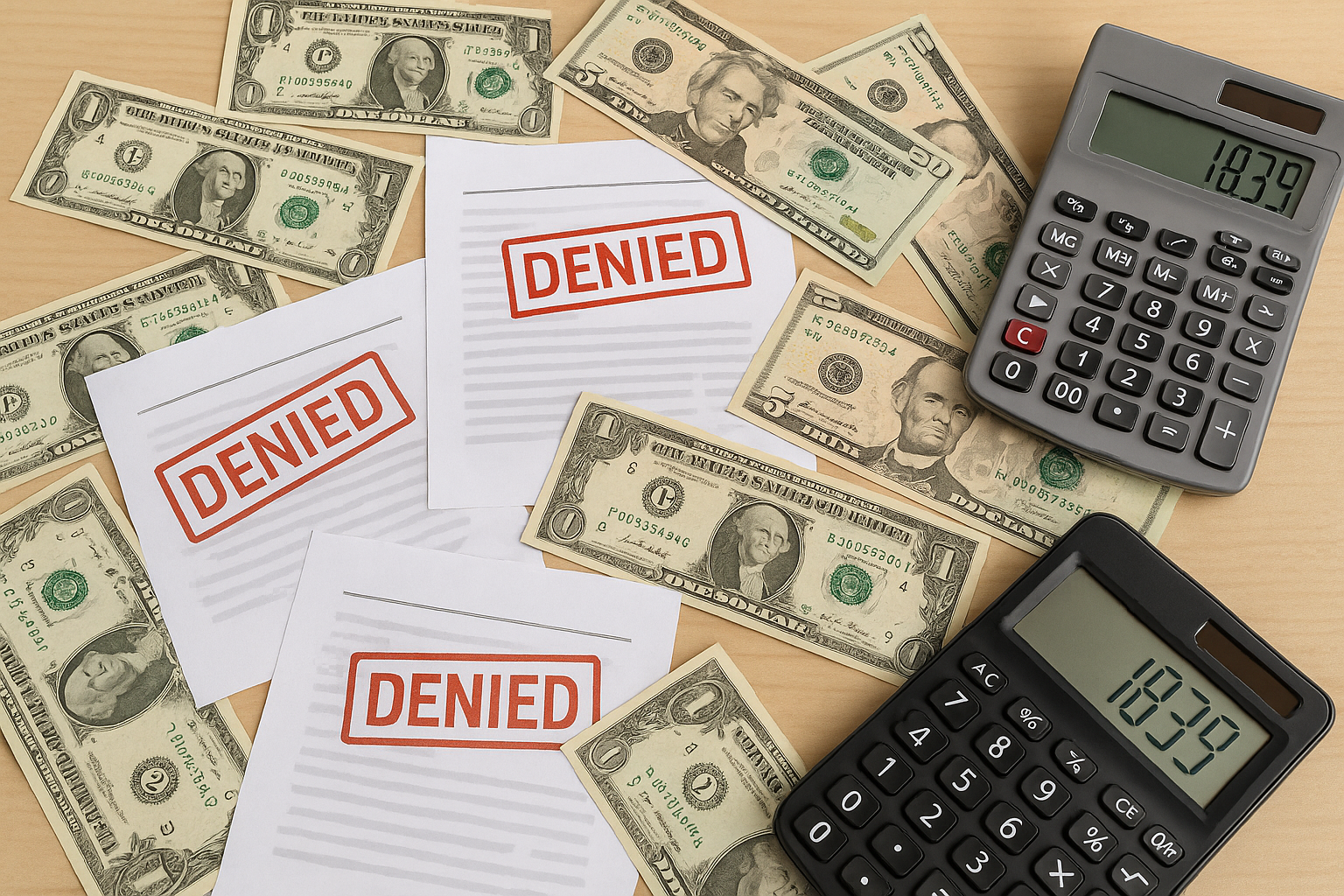
It’s easy to focus your team’s energy on the big-ticket denials—high-dollar claims that demand attention. But while those denials are obvious, what’s often overlooked are the low-dollar, low-effort denials that quietly accumulate and slowly drain your revenue. The $15 here, the $42 there—they may seem insignificant in isolation, but across a month or quarter, these…
-
🏔️ Authorization Avalanche: Reducing Workflow Bottlenecks in Prior Authorization

The Prior Auth Problem Isn’t Going Away If you feel like getting a prior authorization approved takes longer than delivering care—you’re not alone. Payers are expanding PA requirements across diagnostics, radiology, physical therapy, surgical consults, and even standard medications. As a result: And most dangerously? Claims get denied when PAs aren’t filed—or not filed fast…
-
EHR Blindspots: The Charge Capture Gaps You Didn’t Know You Had

Your EHR system may seem like it’s catching everything—but in reality, silent revenue leaks happen every day. Missed charges, incorrect modifiers, unbilled services, and documentation mismatches can slip through even the most advanced systems when human workflows and EHR functionality aren’t perfectly aligned. The truth is, charge capture isn’t just about clicking the right boxes.…
-
⏳ Silent Denials: When Payers Don’t Respond and A/R Explodes
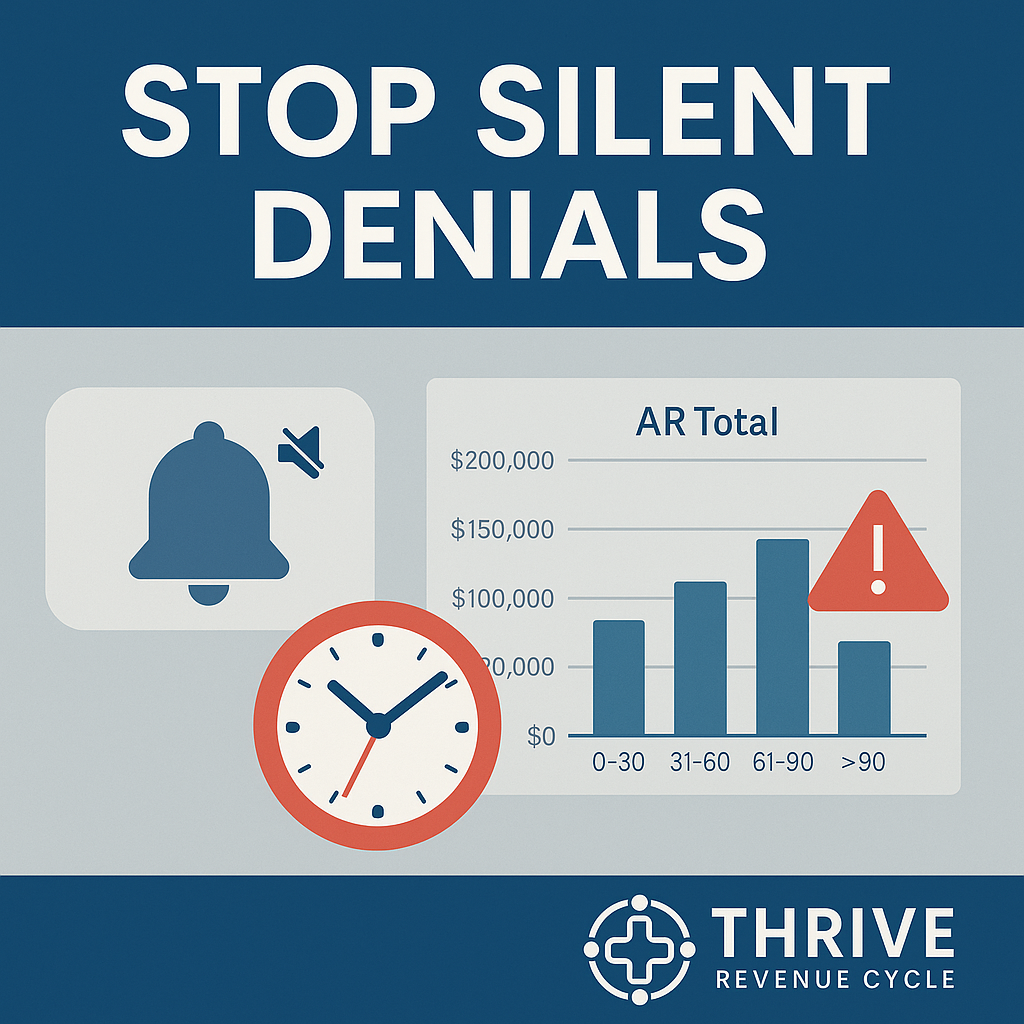
What Are Silent Denials? Unlike formal denials that generate an Explanation of Benefits (EOB) or denial code, silent denials happen when payers simply don’t respond.The claim isn’t processed, isn’t rejected, and isn’t marked as pending. It just… sits there. Why? Silent denials are dangerous because they: The True Cost of Non-Response Every week that a…
-
Portal Paralysis: When Too Many Payer Tools Create More Confusion Than Clarity
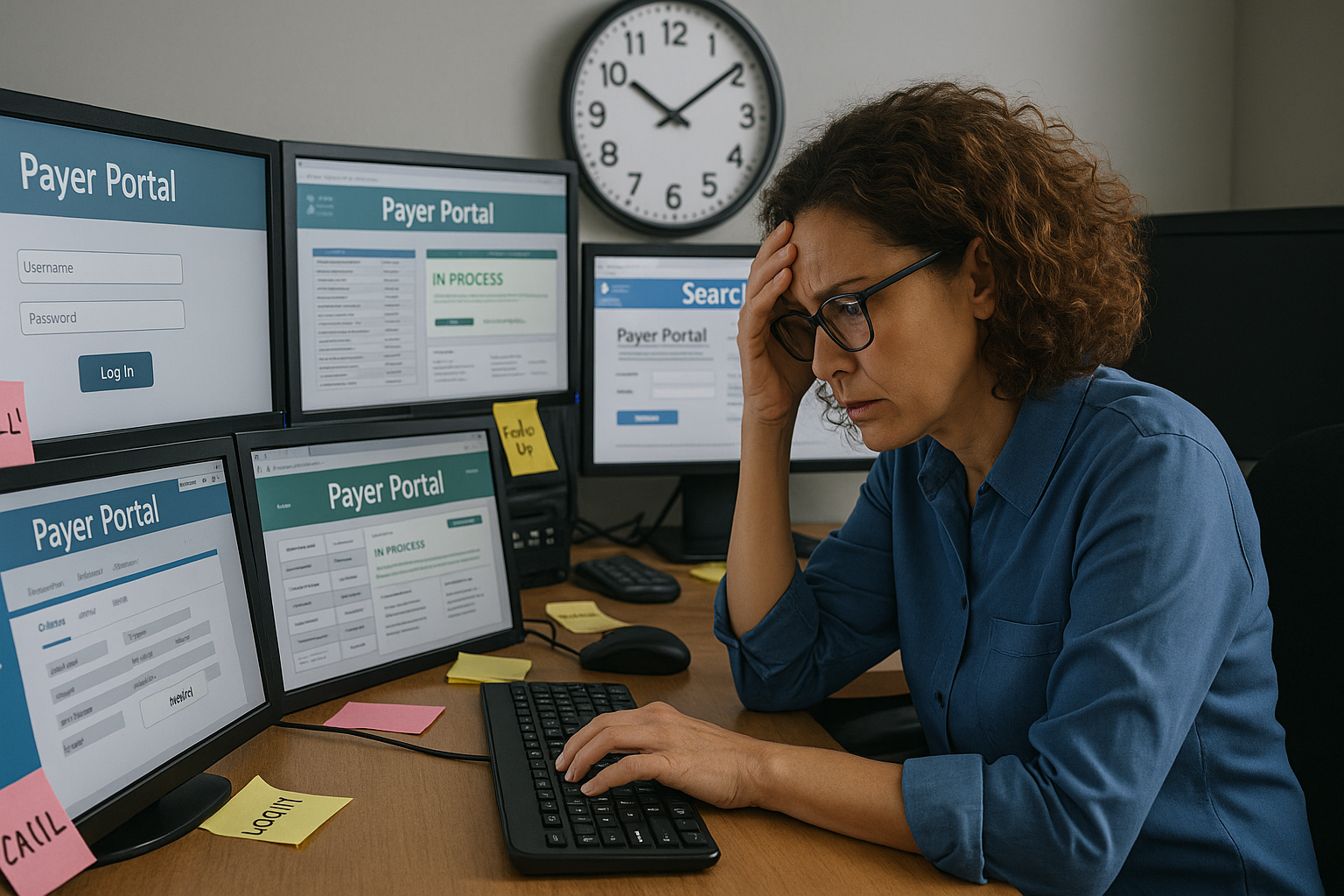
Payers promise transparency and efficiency through their online portals, APIs, and dashboards—but the reality for billing teams is often the opposite. Rather than streamlining workflows, the proliferation of payer-specific tools creates friction, data silos, and duplicated effort. The result? Portal paralysis—when your team is logging into dozens of systems a day, but still not getting…
