Your cart is currently empty!
🛡️ The Denial Shield
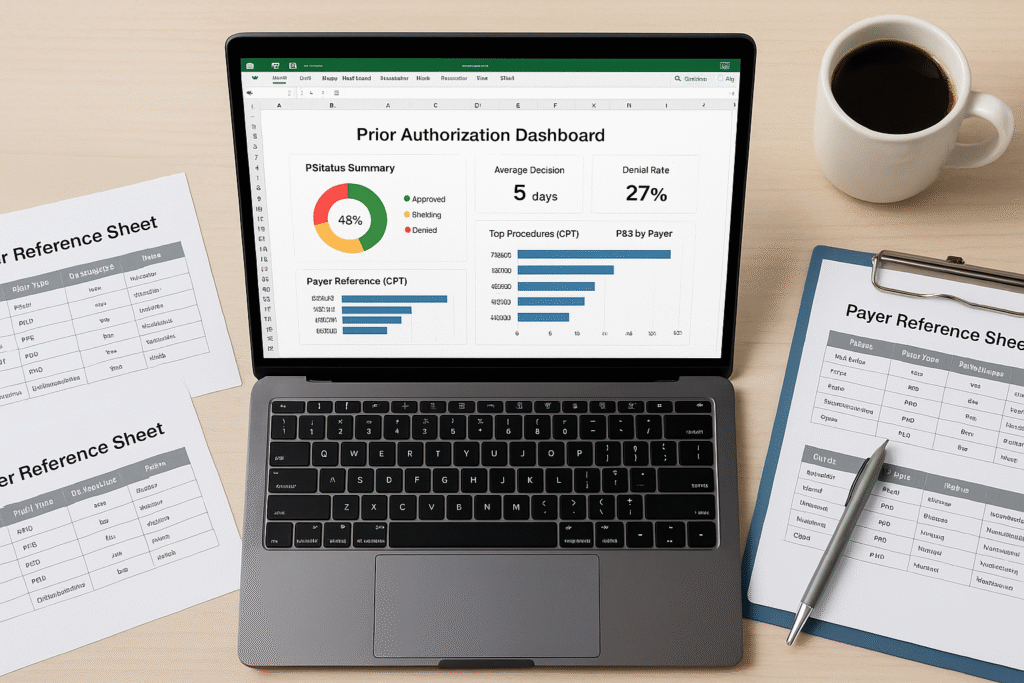
Prior Authorization Intelligence Toolkit
Win More Approvals. Prevent More Denials.
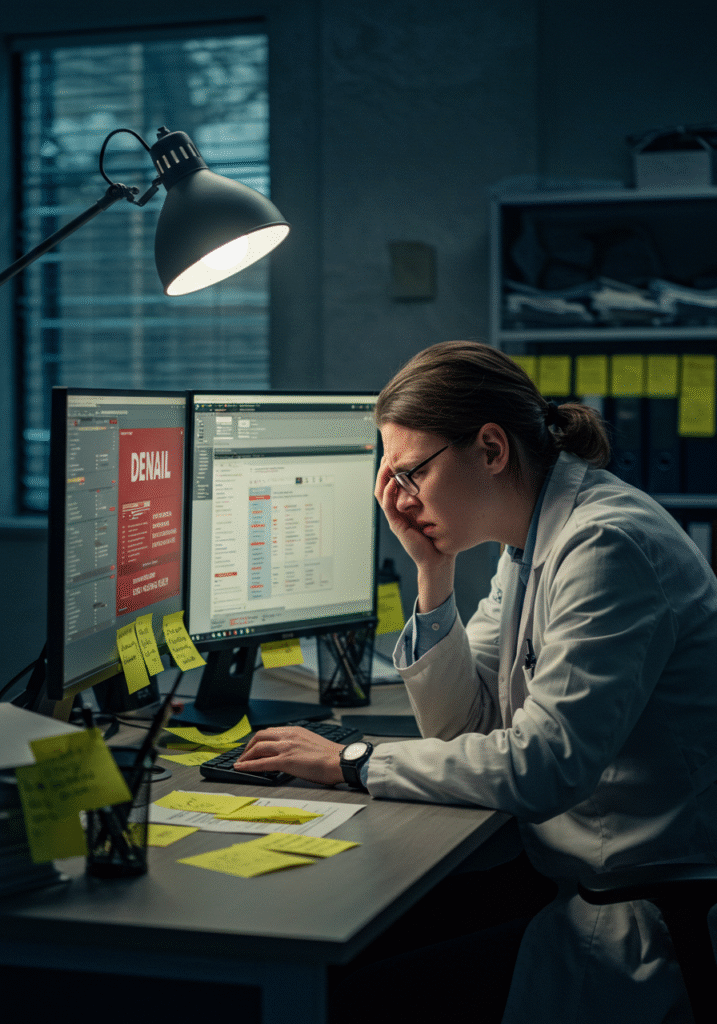
Prior authorization shouldn’t feel like a shot in the dark.
If you’re constantly battling CO197 denials, repeating payer calls, or losing revenue because a form was missing, you’re not alone. The Denial Shield™ gives you the structure, insight, and real-world tools to conquer your prior auth process—before it becomes a denial problem.
📉 Turn prior auth chaos into claim confidence—with intelligence built for busy RCM teams.
👩⚕️ Built for Teams That…
- Are losing time and revenue to CO197 or CO198 denials
- Struggle with payer-specific prior auth rules and fax black holes
- Depend on 1–2 staff who “just know how it’s done”
- Receive late denials after services have already been rendered
- Want to stop relying on guesswork when submitting authorizations
🔧 What’s Included in the Toolkit
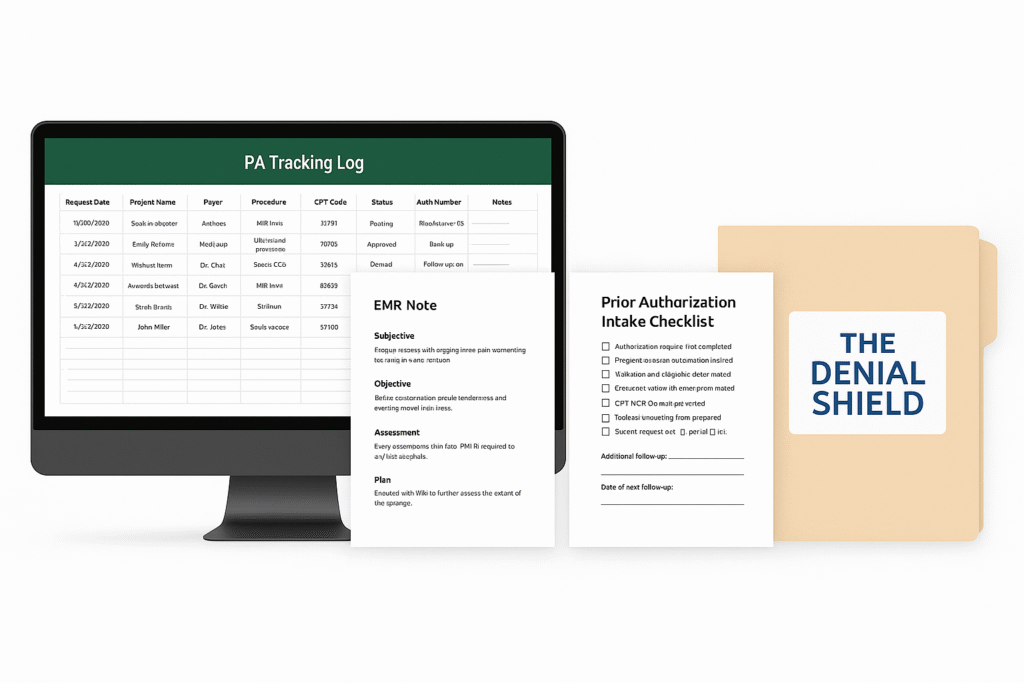
| Component | Description |
|---|---|
| 🧠 Prior Auth Pattern Map | See top denial reasons by payer and service type (built from real-world claim data) |
| ✅ Standardized Authorization Checklist | Customizable, step-by-step checklist for MA, billing, or scheduling staff |
| 📋 Universal Prior Auth Request Template | Adaptable form covering key clinical, service, and CPT data to reduce rejections |
| 🗂️ Payer Contact & Escalation List | Go beyond “call customer service”—access real-world escalation pathways |
| 🔄 Appeal Shortcut Guide | Template letters and timing reminders for when auths are denied or delayed |
| 🧩 Implementation Guide | “Plug-and-play” rollout steps for clinics of any size or staffing model |
📈 Why It Works
- Eliminates blind spots with standardized workflows
- Reduces denials with payer-aware submission guides
- Saves time with ready-to-use templates and contact sheets
- Builds team confidence through clear roles and procedures
- Protects revenue from preventable auth failures
Stop saying “we submitted it” and start showing “we got it approved.”
💼 Perfect for:
- RCM leaders in small-to-mid specialty clinics or rural providers
- Admin staff managing authorizations without formal training
- Groups adding new services or payers needing new auth processes
- Billing teams overwhelmed with back-end denials due to auth gaps
✨ Before & After
| Before The Denial Shield | After The Denial Shield |
|---|---|
| “We’re still waiting on that auth.” | “Submitted on time, correctly, and tracked.” |
| Manual intake steps vary by staff | Standardized checklist used at scheduling |
| Unknown payer rules cause chaos | Reference sheets and tracking logs at your fingertips |
| Denials cost time, money, and staff morale | Clean claims and smoother billing follow-up |
🛠️ Toolkit Pricing
| Version | Description | Price |
|---|---|---|
| Standard Toolkit | All templates, checklists, contact lists, and guides | $325 (one-time) |
| Toolkit + Coaching Call | Includes everything above + 45-minute consult to customize and optimize | $495 |
📥 Delivered instantly in editable formats + printable PDFs
Need a full denial strategy?
Upgrade to 📉 The Denial Impact Map™ or 📊 Denial Strategy Partnership™ to take your clean claims even further.
Includes all tools + instant delivery in editable formats.
Book your 45-minute strategy call to personalize your prior auth process.
